Directory:
Tags:

In 2002 and 2003 two significant US studies suggested that oestrogen, which is standard hormone replacement therapy (HRT), triggered breast cancer and doubled a woman's risk of the disease. As a result, HRT usage fell by a half and thousands of women suffered the debilitating effects of menopause.
According to Cancer Research UK, this drop coincided with a fall in the incidence of breast cancer.
Women dying needlessly
Tamoxifen is a widely used drug for the treatment of breast cancer. It works by blocking oestrogen and is usually given to women after surgery in an attempt to prevent the recurrence of the disease.
According to a 2013 article in The Lancet, tamoxifen and three similar drugs, reduce the incidence of breast cancer by 38% in women at an increased risk of the disease. Although tamoxifen is a lifesaving drug, it has significant side effects, including depression, blood clots, nausea, headaches and exhaustion.
A prescribed course of tamoxifen treatment is usually for five years. Women are failing to complete their courses and are dying needlessly.
A new HRT drug might prevent breast cancer
At the 2013 conference of the American Society for Reproductive Medicine in Boston, Professor Richard Santen from the University of Virginia and an expert on the role of oestrogen in breast cancer, presented findings, which suggested that the earlier US studies were flawed and a new FDA approved Pfizer HRT drug, Duavee, may actually help to prevent breast cancer.
Duavee contains bazedoxifene, which blocks the cancer causing effects of oestrogen, which means that it has the benefits of reducing the symptoms of menopause as standard HRT, but doesn't trigger cancer.
Some facts
Breast cancer is the most common cancer among women in England, accounting for 31% of all newly diagnosed cases of cancer in females.
Over the past 40 years there's been a 38% decrease in breast cancer mortality rates, but the incidence rates of the disease have steadily increased. Each year in the UK, around 50,000 women are diagnosed with breast cancer and each year, 12,000 women in the UK die of it.
Risk factors
Although breast cancer can develop for no apparent reason, there are certain risk factors which increase the chance that the disease will develop. These include: age, where you live, family history, being childless or having your first child over 30, not having breast fed, early onset of periods, continuously taking HRT and excessive consumption of alcohol.
Age is the strongest risk factor and breast cancer rates are climbing among older women. However, cases among younger women are increasing too. Each day in the UK, there are 27 new cases of the disease diagnosed among women under 50.
Wealthier nations have a higher incidence of the disease. The UK has the 11th highest incidence rate and Belgium has the highest incidence of breast cancer in the world.
About 5% of all cases of the disease are caused by a faulty gene, which can be inherited. The genes BRCA1 and BRCA2 are the most common. Scientists continue to explore mutations of these genes, but are also researching how more common gene variations may influence breast cancer risk.
Over 40% of breast cancer in the UK is preventable
In recent years, studies have examined the potential impact of environmental factors on the disease: the effects of exercise, weight gain and loss and diet.
According to the World Cancer Research Fund, 42% of all cases of breast cancer in the UK are preventable. Women who are overweight or obese are at a higher risk. Studies show drinking just one large glass of wine a day increases the chances of developing the disease by 20%.
The National Institute of Environmental Health Sciences in the US is funding a 10 year sister study designed to examine the possible causes of the early onset of breast cancer. Comprised of 50,000 women who have sisters with breast cancer, the study will collect information about genes, lifestyle, and environmental factors that may cause breast cancer.
New diagnostic tests
In time, 3D breast tomosynthesis is expected to replace conventional mammography. This is an extension of the digital mammogram and combines low-dose X-rays of the breast with 3D imaging technology in the expectation of obtaining a more in-depth view of breast tissue.
The Cleveland Clinic in the US hailed the FDA-approved 3D techniques as one of the top 10 medical innovations for 2013. A new study published in Lancet Oncology found that by adding 3D digital breast tomosynthesis to the standard 2D breast X-rays could reduce results that look like cancer, but are not, by 17%, without missing any cancers.
Aixplorer is a new FDA approved ultrasound 3D imaging system that could reduce unnecessary biopsies by helping to detect which lumps are malignant. Twenty per cent of women who have breast biopsies prove negative for cancer. The Aixplorer measures tissue stiffness, which is more prone to be cancerous. The technology's 3D images could also be helpful for screening younger women with denser breast tissue for cancer, since traditional mammography doesn't work so well in such patients.
A molecular breast imaging test in development, scintimammography, entails injecting a mildly radioactive tracer into a vein that attaches to breast cancer cells and can then be detected by a camera. The procedure detects early signs of breast cancer and explores suspicious areas detected by regular mammograms. Early studies suggest that scintimammography may be as accurate as the more expensive MRI scans.
Targeted therapies
As researchers have learned more about the gene changes in cells that cause cancer, they have been able to develop newer drugs that specifically target these changes. Such drugs are transforming the way cancer is treated.
The most well known targeted therapy is trastuzumab, which is marketed as Herceptin. Herceptin targets breast cancers that express high levels of HER2. Known as HER2 positive cancers they account for some 20% of all breast cancers.
Targeted therapies work differently from standard chemotherapy and often have different and less severe side effects such as sickness and hair loss. Targeted therapies have begun to make personalised medicine a reality and will continue to help clinicians tailor cancer treatment based on the characteristics of each individual's cancer.
Takeaway
Researchers from the Cleveland Clinic have discovered a single vaccination that can prevent cancer in mice that are genetically predisposed to the disease. Clinical studies in humans are expected to begin in 2015. The first study will include women with aggressive breast cancer who have recovered from standard treatment. A second study will include healthy women, such as Angelina Jolie, who have undergone mastectomies to lower their breast cancer risk.

|
|
|

Traditional marketing for GPs is dead and a waste of money.
The information age has shifted the balance of power from GPs to patients. Today, patients use social media to share information about health providers at lightning speed, 24-7: 365 days a year and doctors can't stop it.
More telling is the fact that 35% of all patients who use social media say negative things about doctors, 40% of people who receive such negative information believe it and 41% say it affects the choices they make. Social media is the new frontier of reputation risk for doctors.
Some facts
According to a number of recent surveys, 84% of US health providers have Facebook pages, 64% have Twitter accounts, 46% post videos on YouTube, a significant percentage have profiles on LinkedIn and 12% blog. These data are indicative of what's happening in the UK. However, because doctors increasingly participate in social media doesn't mean that they are using it optimally.
Few doctors understand how social technologies interact with patients. Few use social media to reduce negative patient conversations, increase referrals, expand their services, enhance their reputations, drive loyalty and increase revenues. There are at least three reasons for this:
- Although patients increasingly engage in social media conversations, doctors don't know how to influence these
- Doctors tend to define social media technically and fail to leverage the behavioural aspects of the medium, which facilitate faster, cheaper, easier and larger scale social interactions than before
- There is no single measure of social media's financial impact, and therefore doctors find it difficult to justify allocating resources to an activity whose precise effect remains unclear.
Reputations defined by patients
Thirty three percent of all patients use social media to seek medical information, track symptoms and broadcast opinions about doctors, drugs and treatments. Age is a factor: 50% of seniors; 45% of 45 to 65 year olds and 90% of 18 to 24 year olds use social technologies to do these things. Ninety percent of everyone who uses social media trusts the health information they receive.
Although it's difficult to quantify the impact that social media has on health providers, we know that patients use social technologies throughout their entire therapeutic journeys to form opinions and help them make critical choices.
Being visible is being credible
Increasingly, patients are using social networks to obtain answers to healthcare questions and to research disease states. If a health provider has a poor internet presence, patients will question their services and expertise. A weak website with poor information will trigger huge numbers of negative conversations that tarnish reputations.
Being visible is made difficult by the size and structure of the online health market. There are over two billion websites dedicated to health in an unregulated and fragmented global marketplace. This, not only makes it difficult for health providers to gain visibility, but it frustrates and confuses patients seeking health information, which impacts on the doctor-patient relationship.
Video has become the preferred format of consumers to receive health information. Also internet browsers put a high premium on video content, so websites that use video appear higher in search hierarchies and are more appreciated by patients.
Provide what patients' want
Seventy percent of patients who search online for health information want specific answers to FAQs about disease states: symptoms, diagnosis, treatments, side effects and aftercare. Patients want access to health information at speed from anywhere, any time and anyhow. Smartphones are fast becoming the gateway to health information.
Patients prefer health information in video format because it delivers a human-touch that digitalized written words don't.
Elevate the role of patient insights
Generating rich patient insights is challenging, but important. Doctors can use social media to "listen" to patients across a few, but significant touch points of their therapeutic journeys and respond quickly to signs of changing patient needs. And this can be achieved at much less cost than what traditional communications would cost.
The power and utility of social technologies hinges on participation of both health providers and patients, which suggests flatter and more responsive organisations. Creating these is challenging. And less hierarchical and more responsive organisations should not mean diminished accountability.
Boost productivity
The behavioural aspects of social media provide doctors opportunities to organise healthcare differently. For instance, using social technologies internally to communicate with colleagues transforms messages into content, which increases the efficiency of searching and results in faster and more effective collaboration.
Doctors can employ social technologies to create data and information collaboratively, which is more accurate and valuable than that collected by more traditional methods.
Takeaway
Using social media to create, develop and manage online communities of patients, payers, specialists etc can yield significant benefits for GP practices. Over time, such communities can be used to enhance patient care, respond to patients' changing needs, amplify and broadcast new services and expertise and encourage changes in the behaviour and mindsets of patients and other stakeholders.

Here's the paradox: cancer is the most preventable of all the chronic illnesses and yet the incidence of cancer growth in Africa and other developing regions of the world is of pandemic proportions, which is exacting a significant economic and social toll.
Reason 1: There is a massive difference between global spend on cancer and on infectious diseases. Although cancer claims more lives globally than HIV/AIDS, malaria and tuberculosis combined, it receives less than three percent of public and private funding from global health. The overwhelming amount goes to infectious diseases.
Reason 2: African countries lack financial clout to attack cancer. They lack epidemiological information to guide resource planning. They lack health workers. They lack the political will and they have competing healthcare demands.
Reason 3: Bad advice. For example, recently a well resourced UK global health advisory group travelled to a poorly resourced African country, which had one of the world's highest rates of cervical cancer mortality and recommended that it should improve its road transport infrastructure to enable health workers easier access to rural areas.
Narrowing the global medical knowledge gap
Sixty years ago, cervical cancer was one of the most common causes of death for western women. However, between 1955 and 1992, the cervical cancer mortality rate in affluent western countries declined by almost 70% as medical knowledge to detect and manage the disease improved. Similar outcomes are true of other forms of cancer to the point where cancer is now preventable and manageable in most developed economies.
According to Margaret Chan, Director General, World Health Organization, the exponential growth of cancer in Africa can be significantly reduced and managed by narrowing the medical knowledge gap between the develop world and African countries.
Notwithstanding, well resourced dedicated centres of global health in affluent developed countries are failing to narrow this gap and thereby failing to reduce and control the 12 million cancer cases that occur annually. If this gap continues over the next 20 years, cancer is expected to exact a significant toll in morbidity, mortality and economic cost particularly in Africa. By 2030, the number of new cancer cases each year is projected to increase to 27 million, cancer deaths to 17 million and much of the cancer burden will fall on poorly resourced African countries.
Mobile phones rather than tarmac
Narrowing the medical knowledge gap between rich and poor countries will neither be achieved by building more roads nor continuing traditional ways of communicating medical knowledge. Such means are slow, costly and ineffective. Narrowing the medical knowledge gap will only be achieved by widespread use of the most ubiquitous healthcare innovation: the mobile telephone.
Although operationally relevant, the mobile telephone is an underdeveloped healthcare application. However, in Africa, the implementation of any healthcare strategy to reduce the burden of cancer and other debilitating health conditions should not be contemplated without leveraging mobile telephony. Why? Because Africa has one of the fastest growing telecommunication infrastructures in the world.
According to a recent joint World Bank and African Development Bank Report there are 650 million mobile users in Africa, surpassing the number in the US and Europe. "In some African countries more people have access to a mobile phone than to clean water, a bank account or electricity," the Report says.
A recent Deloitte's Report suggested that between 2000 and 2012, mobile phone penetration in Africa increased rapidly from one percent to 54%. Today it is over 60%. The main catalyst for this explosive growth is youth. "The cell phone is their landline, ATM and email in one device. Cell phones are central to their life," says Teresa Clarke, CEO, Africa.com.
According to Maurice Nkusi from Namibia Polytechnic who designed a mobile phone-based curriculum, most African youths, "have never even used a computer, but the rapidity with which they master mobile telephony reflects the era in which they live".
Mobile telephony in Africa has narrowed divides between urban and rural, rich and poor and African youth today is the first generation to have direct access to mobile phones, which are used for communicating, transferring money, shopping, listening to the radio and mingling on social media. It is a relatively small step to integrate healthcare content on mobiles that would help prevent and manage cancer.
Africa internet use increases as costs fall
Internet prices in Africa are falling and speed is increasing thanks to fibre-optic submarine cables running along the east and west coasts of Africa and connecting many countries and millions of people.
The Eastern Africa Submarine Cable System (EASSy) is a 10,000km fibre-optic cable deployed along the east and south coast of Africa to service voice, data, video and internet needs of the region. It links South Africa with Sudan via landing points in Mozambique, Madagascar, the Comoros, Tanzania, Kenya, Somalia and Djibouti. The system also interconnects with multiple international submarine cable networks for onward connectivity to Europe, the Americas, the Middle East and Asia.
At a 2013 BRIC summit in South Africa, Andrew Mthembu, chairman, i3 Africa announced that EASSy is to be complimented by a new marine cable connecting 21 African countries with Brazil, Russia and China.
Along the West African coastline is a similar submarine fibre-optic cable, which links West African countries with Europe and brings ultra-fast broadband to a region from Seixal in Portugal through Accra in Ghana to Lagos in Nigeria and branches out in Morocco, Canary Islands, Senegal and Ivory Coast.
This existing 7,000km cable has been recently complemented by a France Telecom-led system, which uses high-speed fibre optic technology to link Europe with 18 countries along the west coast of Africa and provides the capacity to allow approximately 20 million ordinary videos and up to five million high definition videos to be streamed simultaneously, without any buffering.
Today, there are 84 million Internet-enabled mobiles in Africa, all of which can access data and rich media from the internet. By 2014, 69% of mobiles will have Internet access in Africa. In response to the burgeoning demand, African markets are rapidly transitioning from mobiles with limited data access to low-cost smartphones with access to the Internet. Chinese handsets are readily available in Africa for as little as US$20.
Takeaways
Previous HealthPad commentaries have described mHealth initiatives in Africa, but few western centres for global health have fully appreciated that medical knowledge has become mobile, digital and global. Further, they have not fully appreciated the telecommunications revolution that has taken place in Africa over the past decade. Such failures help to explain why the medical knowledge gap between the developed world and African countries has not been narrowed.
This failure is also an opportunity for centres of global health to take a lead in capturing and organising medical knowledge to assist in the management of cancer and other chronic diseases and then to leverage established telecommunications infrastructures to distribute that knowledge to where it is needed the most. What a pity that narrowing the medical knowledge gap was not a Millennium Development Goal.

|
In 2010, tennis legend Billie Jean King had both her knee joints replaced and it changed her life. Years playing the high-impact sport left the 39-time Grand Slam winner with joint pain and stiffness in her knees. Now at 68, she is playing tennis again. Like Billy Jean, thousands of people are opting to replace their traumatised joints and patients are fast becoming younger.
An escalating incurable and costly condition As populations age peoples' joints are increasingly affected by osteoarthritis, a painful and incurable condition. Dr Anestis Iossifidis consultant orthopaedic surgeon, Croydon University Hospital, UK, says, "Osteoarthritis is the most common disease of the joints and one of the most widespread of all chronic diseases and the most common cause of severe long term pain and physical disability". At any one time, 30% of American adults are affected by joint pain, swelling, or limitation of movement. The prevalence of osteoarthritis increases markedly with age and by 65 can be observed in over half of the American population. Worldwide an estimated 630 million people have their lives blighted by osteoarthritis. In the UK the disease affects about 8.5 million people; a figure set to double to 17 million by 2030. The condition forces 33% of sufferers to retire early and each year this is estimated to cost the UK economy £3.2 billion. |
|
|
|
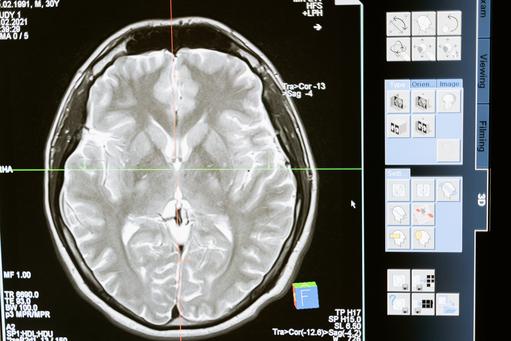
Two years ago, Ben Brabyn, a forty year old former British Royal Marine and investment banker turned entrepreneur, visited his doctor with headaches that another doctor had diagnosed as sinusitis. The second doctor suspected a brain tumour and immediately called for an ambulance to take Ben to Charing Cross Hospital, London. Scans showed a fist-sized tumor on the right side of his forehead, see above. Undetected, Ben's tumor could have killed him within days
Any brain tumor is serious and life-threatening because of its invasive nature in the limited space of the intracranial cavity. The threat a brain tumor poses depends on its type, invasiveness, location, size and the state of its development. A tumor may be particularly deadly because it can push against or invade important parts of the brain, as well as cause a lot of swelling that can result in blackouts, fits and other serious health challenges. Within hours of being admitted to hospital, surgeons removed a large panel of bone over Ben's right eye and excised his tumor, which turned out to be a benign meningioma. Most meningiomas are benign and tend to be more common in middle-aged or elderly women than in men. Ben is now fully recovered. Brain tumor deaths are increasing Each year, around 165 million people in Europe are affected by some form of brain-related disorder, which suggests that almost every family in Europe is likely to be affected. Not everyone however will be as lucky as Ben Brabyn. In the US, over 688,000 people are living with primary brain tumors, some 138,000 are malignant and about 550,000 are non-malignant. Since 2004 the incidence of brain tumors in the US has increased by 10%. In 2013 in the US, an estimated 70,000 new cases of primary brain tumors are expected to be diagnosed. In 2012 an estimated 13,700 deaths were attributed to primary brain tumours. Brain tumors are the second-leading cause of cancer deaths in American children. In 2013, approximately 4,300 Americans younger than 20 will be diagnosed with primary brain tumors. In the UK the situation is equally bleak. Over 9,000 people are diagnosed with brain and spinal cord cancer annually and it kills nearly 5,000. Over the past decade there has been a 16% increase in brain tumor deaths. The largest group of primary brain tumors is gliomas; a broad term that includes all tumours arising from the gluey supportive tissue of the brain. These make up 30% of all brain and spinal cord tumors and 80% of malignant brain tumours. |
|
|

|
|
|
|

|
|
|

|
|
|
|
In January 2013 Andrew Marr, the 53-year-old BBC TV presenter and journalist, had a stroke after a bout of intensive exercise on a rowing machine in a gym. What is a stroke? A stroke is a serious medical emergency where the supply of blood to the brain is disrupted. In over 80% of cases, strokes usually happen because a blood clot blocks the blood supply to the brain. They can also happen when a weakened blood vessel that supplies the brain bursts and causes brain damage, known as a haemorrhagic stroke. Andrew Marr's stroke prompted two questions: (i) Do younger healthy people have strokes? and (ii) Does physical exercise contribute to strokes? Are stroke victims getting younger? Andrew Marr was one of 152,000 people in the UK who have strokes each year. Stroke is the third largest cause of death in the UK and the largest single cause of severe disability. There are approximately 1.1 million stroke survivors living in the UK and each year strokes cost the NHS £2.8 billion. The picture is no better in the US, where every 40 seconds a person has a stroke, each year strokes kill 130,000 and cost the US $38.6. Strokes are uncommon, but not rare in men in their fifties like Andrew Marr. Recent research suggests that strokes among the elderly are declining, while strokes among younger people are increasing. Between 1998 and 1999 in the UK, 9,000 people under 55 were admitted to hospital due to stroke. By 2011 this figure had risen to more than 1,600. It is not altogether clear why stroke is increasing among younger people, although experts note its correlation with type 2 diabetes. The importance of specialist stroke units Andrew Marr said that he believed what he read, that taking, "Very intensive exercise in short bursts is the way to health." Just before his stroke he said, "I went onto a rowing machine and gave it everything I had and had a strange feeling afterwards: a blinding headache and flashes of light". He took no notice and went home. The following morning he woke up lying on the floor unable to move. The most important care for people with any form of stroke is prompt admission to a specialist stroke unit, but even with prompt treatment a stroke can often be fatal. |
|
|





