Dr Thimappa Hegde is the Director of the Narayana Institute of Neurosciences.
After training in Neurosurgery at the prestigious National Institute of Mental Health and Neurosciences (NIMHANS), Bangalore, he served as the faculty of NIMHANS and rose to the position of Additional Professor of Neurosurgery. He worked in NIMHANS for over 20 years during which he was instrumental in initiating Stereotactic and Functional Neurosurgery. He also did a fellowship in skull base surgery in Washington D.C.
Dr. Hegde has performed several thousand Neurosurgical procedures. He has authored 30 scientific publications in leading journals and has contributed chapters to a book on the history of neurosciences. Recognized by the Lions Club of Bangalore as an ‘Outstanding Citizen’, he visited USA and Canada on a special exchange program from the Rotary International. He was invited by the Vatican to speak at an International Meeting at the Vatican City and had a special audience with the POPE - His Holiness John Paul II.
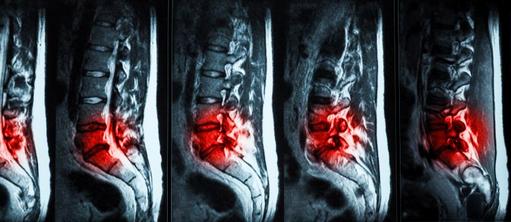
Dr. Hegde's interests include Stereotactic and Functional surgery, Spinal surgery and fusions, Neurotrauma, Neuro-endoscopy and Neuro-oncology.