Directory:
Tags:

|
Public smoking bans and eating fibre significantly reduces people attending hospitals for asthma. These are the conclusions of two 2014 studies: one reported in the Lancet and the other in Nature Medicine.
Asthma Asthma is the inflammation of the air passages in the lungs. It occurs when the immune system mistakes harmless triggers, such as dust mites as threats, which cause the airways to become inflamed, leading to symptoms such as wheezing and breathlessness. Worldwide the economic costs associated with asthma exceed that of TB and HIV/AIDS together. |
|
|
|
|
|
Directory:
Tags:

|
Cataract surgery, once only for elderly patients, is now increasingly being performed on younger baby boomers.
Facts More than half of the over-65s suffer from cataracts, which are cloudy patches in the lens that make vision blurred or misty. The condition is linked to smoking, poor diet or health conditions such as diabetes. Cataracts can affect your ability to read, write, watch TV, work at a computer, and drive. Severe cases can affect your ability to wash, dress, cook and work. According to the World Health Organization (WHO), 285 million people worldwide are visually impaired, 90% of these live in developing countries where cataracts are the leading cause of blindness. |
|
|
|
|
|
Directory:
Tags:

Are we addicted to foods that make us obese and kill?
Why is it hard for obese people to lose weight despite the social stigma and health consequences associated with being overweight? Is it similar to cigarette smokers who continue to smoke even though they know smoking will give them cancer and heart disease?
Is processed food the new tobacco?
Large growing global epidemic
Over the past 25 years the prevalence of obesity in England has more than doubled and today, most English people are either overweight or obese. Similarly, in the US more than a third of individuals are obese.
It’s estimated that each year, obesity costs the NHS more than £5bn and the US economy about $150bn.
Global epidemicOnce considered a problem only for rich countries, obesity is a rising worldwide challenge. In 1997 the World Health Organization (WHO) formally recognized obesity as a global epidemic and in 2008, claimed that 1.5 billion adults were obese.
Experts say a couch potato lifestyle and overindulgence in junk food is creating an overweight and obese generation prone to heart disease, diabetes and cancer. In rich countries people have easy access to cheap, high-energy food that is often aggressively marketed.
Call for parents and local authorities to help
The press refers to the “obesity time-bomb” and suggests that misguided parents are bringing up a generation of overweight children who gorge on junk food and sugary treats and rarely get any exercise. UK policy makers say that more should be done to support families to help them tackle the obesity crisis in children and young people.
In January 2014, Professor Philip James told the European Congress on Obesity in Antwerp: “Unless we can act firmly and decisively, we will be condemning a huge number of children . . . to becoming a ‘lost generation’.”
Where should we target our concerns? Parents? Municipal authorities? Or, the food and drinks industry?
Changed environment
Contrary to popular belief, people have not become greedier or less active, but what they eat has changed. Everyday, people are bombarded by food industry adverts to eat more food. New scientific evidence suggests that industrial processed food is biologically addictive.
The tobacco industry
In 1954, the tobacco industry paid to publish a “Frank Statement to Cigarette Smokers” in hundreds of US newspapers. It stated that the industry was concerned about peoples’ health and promised a number of good-faith changes.
What followed were decades of deceit and actions that cost millions of lives. During that time the tobacco industry emphasised personal responsibility and paid scientists to deliver research that triggered doubt and criticised science that found harm associated with smoking.
The food and drink industry
Similarly today, some large food and drink companies fund scientific research to establish health claims about their products.
A 2013 report suggests that scientific research sponsored by the food and drink industry is five times more likely to conclude that there are no links between consumption of sugary drinks and weight gain.
In March 2014, Dame Sally Davies, the UK’s Chief Medical Officer told a committee of MPs that, "research will find sugar is addictive" and that the government, “may need to introduce a sugar tax".
For years the tobacco industry made self-regulatory pledges, aggressively lobbied to stifle government actions and denied both the addictive nature of tobacco and their marketing to children.
Takeaways
Food and tobacco industries are different, but there are significant similarities in the actions they have taken in response to concerns that their products can harm.
Because obesity is now a pandemic the world cannot afford to make the same mistake it did with the tobacco industry.
Directory:
Tags:
|
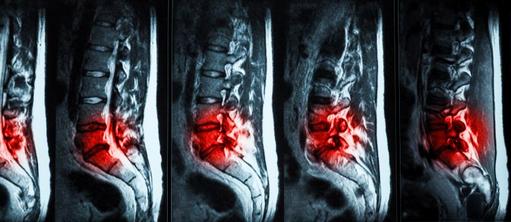
Herniated disc surgery is the "bread and butter" for spine surgeons, but might not remain so. In the developed world, populations are rapidly aging, comorbidities are changing and the number of spine surgeons is shrinking.
Herniated disc A herniated or slipped disc is where one of the discs in the spine ruptures and the gel inside leaks (herniates) and causes back pain and sciatica. Once the nucleus herniates, pain in the lower back may improve, but sciatic leg pain increases. This is because the jelly-like material puts pressure on spinal nerves, which causes pain, numbness, or weakness in one or both legs. |
|
|
|
|
Directory:
Tags:

|
In October 2013 Professor Olaf Wendler, Clinical Director of Cardiology and Cardiothoracic Surgery at King's College Hospital London performed a new surgical heart procedure for the first time in the UK called less invasive ventricular enhancement or LIVE.
New procedures better for an aging population The path breaking operation uses a new device, developed by Bioventrix, Inc. that enables surgeons to effectively "exclude|" scarring. The procedure involves re-modelling the patient's left ventricle, which is the part of the heart responsible for pumping oxygen rich blood to the body, whist the heart is still beating. It's particularly suitable for elderly frail patients suffering from chronic heart disease and the benefits include small incisions, faster recovery and better outcomes. With traditional open-heart surgery the surgeon makes a ten to twelve-inch incision and then gains access to the heart by splitting the breast bone and spreading open the rib-cage. The patient is then placed on a heart-lung machine and the heart is stopped for a period. This approach, inappropriate for frail older patients with advanced heart disease, can be associated with postoperative infection, pain and a prolonged recovery time. |
|
|
|
|

|
A cheap spit-test that reveals the secrets of your genome, used by hundreds of thousands of people worldwide has been stopped by the FDA.
FDA warning letter On November 22nd 2013 the FDA sent a warning letter to 23andMe, a privately held personal genetic-testing firm based in Mountain View, California to, "immediately discontinue" providing its saliva collection kit and Personal Genome Service, because it had failed to provide adequate information to support the claims made in the company's marketing. 23andMe is so named because of the 23 pairs of chromosomes in a normal human cell. Founded in 2006, the Company is a Silicon Valley favourite led by Ann Wojcicki, wife of Sergey Brin, one of Google's founders. It has raised more than US$100 million from backers that include Google, Genentech and Yuri Milner, a billionaire investor in Facebook and Twitter. Taking more control of your health Nature took four billion years to develop the code that determines our life. The Human Genome Project, that ended a decade ago, initiated a medical revolution. In 2003 sequencing an individual genome cost between US$10 and US$50 million. Since then the costs have plummeted towards US$1,000, allowing science and medicine to identify genes with disease causing mutations. In 2008 23andMe's US$99 personal genome test kit was named by Time Magazine as the "invention of the year". |
|
|
|
Directory:
Tags:

|
In 2013, a new surgical procedure was used for first time in the UK at St George's Hospital, London to remove of a cancerous kidney tumour.
The procedure combines the da Vinci surgical system with an injection of a dye into the patient's kidney. The dye illuminates healthy tissue and shows up under the da Vinci's camera as a bright green light and as a consequence the procedure is called Firefly. Chris Anderson, a consultant urologist at St George's is one of the early adopters of robotic surgical techniques after receiving specialist training in 2005 at the world renowned Henry Ford Robotic Center in Detroit. Anderson has built-up a leading renal cancer unit at St George's and introduced the Firefly technology into the UK. He says, "Partial kidney removal is a complex operation that requires complete removal of the tumour and reconstruction of the remaining healthy kidney. By combining the da Vinci system with Firefly we are able to achieve our goal better than in the past". Robotic surgery Kidney surgery is enhanced by robotics. In recognition of the increasing importance of high tech surgical therapies, the N Sethia Foundation funded the UK's first robotic surgery training centre at University College Hospital, London. In pride of place in the new Chitra Sethia Centre for Robotics and Minimal Access Surgery is the latest da Vinci surgical system. |
|
|
|
|
Directory:
Tags:

|
In 2013 the Hollywood actress Angelina Jolie announced that she had both her breasts removed because she carried the BRCA1 gene.
Her bilateral prophylactic mastectomy highlights the fact that a woman whose mother or father carries a faulty BRCA1 gene has a 50% chance of also carrying it and a 60 to 80% higher risk of developing breast cancer. Angelina Jolie exemplifies what many women with a family history of breast cancer are doing: testing for the BRCA1 gene; if positive, electing for a bilateral prophylactic mastectomy and after surgery, reconstructing their breasts. Hollywood myths do women a disservice In a New York Times article, entitled My Medical Choice, Jolie informed women about BRCA gene mutations and the challenges of breast surgery. Her efforts are overshadowed by the notion that breast surgery is quick and easy. Hollywood images propagate the myth that reconstructive surgery quickly restores breast symmetry, improves body image, quality of life, self confidence and wellbeing. In reality, it's major surgery with significant risks that entails an extended series of operations and follow-up visits and can take three to nine months to recover from. |
|
|
|
|

Globally, healthcare is at the centre of a big data boom that may prove to be one of the most significant drivers of healthcare change in the next decade. Today, we're collecting more information than at any point in healthcare history.
In the UK, big data strategy is spearheaded by Health Secretary Jeremy Hunt and NHS England. In the US it is led by the Obama Administration's big data R&D initiative.
American federal health agencies are contributing five-years of public datasets and analytics for genomics and molecular research to a cloud-based research platform hosted by BT. This will compliment the de-identified NHS population, medical and biological datasets that already reside in the cloud.
Failure to deliver
Analyzing these data is expected to enable earlier detection of effective treatments, better targeted clinical decisions, real-time bio-surveillance and accurate predictions of who is likely to get sick. These promises are predicated on the interoperability of the data and the availability data analysts and managers.
According to a 2011 McKinsey & Company Report, "The US alone faces a shortage of 140,000 to 190,000 people with deep analytical skills as well as 1.5 million managers and analysts to analyze big data and make decisions based on their findings".
So far, healthcare systems have failed to deliver on big data promises.
Big data's potential benefits for healthcare
Driving this new open epidemiology research initiative is big data's successes in other sectors and the pressing need to modernise healthcare infrastructure. Like many emerging technologies, the future of big data in healthcare is seen to be full of benefits.
Little data
The promises of big data overlook the challenges of little data. Little data collected at the unit level have two principal challenges: accuracy and completeness.
Insights from data are predicated upon the accuracy and completeness of that data. When data are systematically biased through either errors or omissions, any correlations made are unreliable and could result in misguided confidence or the misallocation of scarce resources.
In healthcare, important clinical data, such as symptoms, physical signs, outcomes and progress notes rely on human entry at the unit level. This is unlikely to change. Health professionals at the unit level will continue to exert discretion over their clinical documentation. Unit level information - little data - presents the biggest challenge for the interoperability within and among healthcare big data initiatives.
Ian Angel, an Emeritus Professor of Information Systems at the London School of Economics uses the North Staffordshire Hospital debacle to illustrate how professionals at the unit level react to data-driven ruled-based management by manipulating data. "Surgeons pushed dying patients out of the operating room into corridors to keep "death in surgery" figures low. Ambulances parked in holding-patterns outside overstretched A&E units to keep a government pledge that all patients be treated within four hours of admission".
Proprietary systems
Big data are most newsworthy, but least effective. Little data are most influential, but least newsworthy.
There are a plethora of technology vendors vying to help a plethora of health providers' to lock-in millions of patients at the unit level with proprietary software systems. Scant attention is given to this.
Further, software vendors predicate their sales on the functionality and format of their systems and data. This obscures the fact that the data format is 100% proprietary. Over time, this cycle of proprietarily locking-in patients at the unit level has created a sclerosis in healthcare infrastructures, which is challenging to unblock. This presents a significant challenge to interoperability and the success of big data.
Errors in little data
Little data documentation can be enabled by technology. For instance, machine learning is a form of artificial intelligence that trains systems to make predictions about certain characteristics of data. While machine learning has proved successful for identifying missing diagnoses, it is of limited use for symptoms and the findings of physical examinations.
Despite technological advances, clinicians' notes remain the richest source of patient data. These are largely beyond the reach of big data.
Another technology, which supports clinical documentation, is natural language processing (NLP). This identifies key data from clinical notes. However, until the quality of those notes improve, it will be challenging for NLP programmes to procure the most salient information. Continued investment in technical solutions will improve data accuracy, but without fundamental changes in how care is documented, technology will have limited ability to rid data of systematic errors.
Incomplete data
Even if we achieve perfect data accuracy, we're still faced with the challenge of data fragmentation. Incomplete data are common in clinical practice and reflect the fragmented nature of our healthcare systems. Patients see multiple health professionals who do not communicate optimally.
Incomplete data, like inaccurate data, can also lead to missed or spurious associations that can be wasteful or even harmful to patient care.
Privacy is less challenging
Solutions to address fragmented data are no easier than those to address inaccurate data. For decades policy makers have pursued greater interoperability between electronic clinical systems, but with little success.
Recent initiatives on interoperability of big data primarily focus on moving specific clinical data, such as laboratory test results, between discrete health providers. This does little to ensure that provider organizations have a comprehensive picture of a patient's care across all care sites.
Privacy advocates are understandably concerned about efforts to aggregate data. However, with adequate de-identification and security safeguards, the risks of aggregation can be minimized and the benefits of better care at lower costs are substantial.
Takeaway
To reap the benefits from big data requires that we understand and effectively address the challenges of little data. This is not easy. But ignoring the challenges is not an option.

NHS maternity units are in crisis because of the shortage of midwives and the increase in births. According to a UK National Audit Office 2013 Report, there's a shortage of 2,300 midwives and births are at their highest level for 40 years. This is straining overstretched maternity units and resulting in closures and blunders.
Closures of maternity units
"Where the demand for maternity services might outstrip capacity, some trusts are restricting access through pre-emptive caps on numbers or reactive short-term closures in order to safeguard the quality of care," the Report says.
Between April and September 2012, 28% of NHS maternity units closed for 12 hours or more, including eight that shut for a total of at least two weeks, either because they lacked physical capacity or midwives.
Health Minister's response
In response to the Report, Dr Dan Poulter, the UK government's health minister, said there were 1,300 more midwives than in 2010 and 5,000 more had been in training since then. The number of midwives in the NHS, he said, was increasing twice as quickly as the birth-rate. Also, the presence of consultant doctors on maternity wards had increased significantly.
Notwithstanding, the National Audit Office report drew attention to the high dropout rate and impending retirements of midwives. This could mean that shortages will continue.
The impact of the rise in fertility
During the 1990s the total fertility rate (TFR) in England and Wales saw a steady decline. Between 2001 and 2008 it gradually increased. Since 2008 the TFR has remained relatively stable, fluctuating between 1.90 and 1.94 children per woman and peaking in 2010.
There is no single explanation for this rise in fertility. Possible causes may include: more women currently in their twenties having children, more older women giving birth, increases in the numbers of foreign born-women who tend to have higher fertility than UK-born women and government policy and the economic climate indirectly influencing individuals' decisions around childbearing.
The impact of migration on maternity units
Between 2000 and 2010 births in England increased by over 114,000: from 572,826 to 687,007. Immigration has played a role in this. Three quarters of the increase in births was to women born outside the UK. Overall, in 2010, over a quarter of all live births in England were to mothers born abroad. The proportion of such births has grown consistently every year since 1990, doubling over the past decade: from approximately 92,000 in 2000 to almost 180,000 in 2010. This represents nearly 500 births on average every day
Although the Minister is right and an increasing number of midwives are in training, their numbers have not kept pace with the overall growth in numbers of births. Before 2010 UK governments permitted high levels of net migration without ensuring that maternity services received adequate staffing.
The majority of mums are satisfied
Although the Report suggests that many NHS maternity units need to improve, most of the 700,000 women who give birth in England each year are happy with the NHS service they receive.
Notwithstanding, over 25% of maternity units were forced to close. The National Audit Office report drew attention to maternity units having to shut temporarily or turn away expectant mothers because of the dearth of midwives and struggle to cope with the current baby boom.
Quality of care compromised
The paucity of trained staff affects the quality of care. In 2011, one in every 133 babies in England was stillborn or died within a week of birth. As the Report suggests, births are also becoming increasingly complex, putting even more demands on midwives and maternity services. Cathy Warwick, CEO of the Royal College of Midwives, said: "We are many thousands of midwives short of the number needed to deliver safe, high quality care. Births are at a 40-year high and . . . show that this is set to continue".
Increase insurance cover
According to the National Audit Office's Report, maternity units fail mothers and babies so often that one fifth of their budgets is now being spent on negligence cases.
Over the past five years, lawsuits involving alleged failings in maternity care increased by 80%. Increased litigation has meant that in 2012-13 almost £0.5bn was spent on malpractice claims because of blunders during labour. This amounts to about 20% of the NHS's total budget for negligence claims, which translates into about £700 per birth being spent on clinical negligence cover.
Absence of consultants
One concern is the lack of senior staff available on maternity units. More than half of maternity units were not meeting the levels of consultant presence recommended by the Royal College of Obstetricians and Gynaecologists. The Report says that while 73% of obstetric units in hospitals had a consultant on duty for at least 60 hours a week, 53% did not provide as much consultant cover as recommended.
Takeaways
Over the coming years, maternity services in England face significant challenges driven by changing demographics, rising birth rates, increasing fiscal constraints and the continuing rise in maternal morbidity rates. In order to maintain high levels of safety, the service will need to change.
Dr David Richmond, president of the Royal College of Obstetricians and Gynaecologists, suggests that: "Although the UK is generally a safe place for women to give birth, we have known for some time that pressure on maternity services is growing . . . More consultants are needed to deal with not only the rapidly increasing birth rate, but the rise in complex pregnancies, with older mothers, maternal obesity and multiple pregnancies at the fore".





