Publications
- All
-
Following
You must log in
before getting
tailored content. -
Interests
You must log in
before getting
tailored content. - Most liked
- Most viewed
Directory:
Tags:

Located on Upper East Side, NYC pediatric dentist Dr. Sara Babich is serving Manhattan and New York City in NY. As a leading pediatric dentistry specialist, Dr. Babich provides the most technologically advanced, safest and time-tested dental treatments for kids and teens.
Pediatric Dental Center in NYC led by the best in class kids dentist Dr. Babich, who is a university and hospital trained in pediatric dentistry. She is committed to providing a comprehensive dental treatment for infants, children, adolescents and special needs kids.
Pediatric Dentistry: Dr. Sara B. Babich, DDS
116 E 84th St,
New York, NY 10028
(212) 988–4070
Web Address:
https://www.nycpediatricdentist.com/
Our location on the map: https://g.page/dr-sara-babich-pediatric-dds-nyc
https://plus.codes/87G8Q2HV+83 New York
Nearby Locations:
Carnegie Hill | Yorkville | Lenox Hill | Upper East Side | Midtown Manhattan
10029 | 10028 | 10021| 10044, 10065, 10075, 10128 | 10022
Working Hours:
Monday: 9AM-6PM
Tuesday: 9AM-6PM
Wednesday: 9AM-6PM
Thursday: 9AM-6PM
Friday: 9AM-4PM
Saturday: Closed
Sunday: Closed
Payment: cash, check, credit cards.
Directory:
Tags:

How Tooth Sealants Prevent Cavities in Children and Teens
Dental sealants are a great way to protect your growing child’s teeth from cavities. Sealants can prevent decay by as much as 80 percent, according to the American Dental Association (ADA.) A relatively recent advance in children’s dentistry, dental sealants for kids teeth help avoid much more costly dental restorations. It’s a win-win!
In our practice we use the latest dental sealants including Silver Diamine Fluoride Treatment (SDF). The Food and Drug Administration has designated silver diamine fluoride with Breakthrough Therapy Status.
What Are Sealants for Kids Teeth?
Dental sealants are protective plastic coatings applied to the chewing surfaces of primary (baby) and permanent (adult) molars to prevent tooth crevices from trapping food particles and bacteria. Sealants are recommended by the ADA and the American Academy of Pediatric Dentistry (AAPD).
How Dental Sealants Prevent Decay?
Sealants act as a barrier to food, plaque and acid to protect the decay-prone areas of the teeth. The back teeth are the ones that are most likely to show signs of decay, so it is important to take this extra step to help protect them.
Sealants are applied when molars erupt beyond the gums, generally between five and 10 years of age. They and are not typically visible when a child laughs, talks, or smiles. While sealants can last for many years, they need to be maintained and evaluated for wear, and occasionally require touch-ups.
Read more: https://www.nycpediatricdentist.com/sealants/
Pediatric Dentistry: Dr. Sara B. Babich, DDS
116 E 84th St,
New York, NY 10028
(212) 988–4070
Web Address:
https://www.nycpediatricdentist.com/
Our location on the map: https://g.page/dr-sara-babich-pediatric-dds-nyc
https://plus.codes/87G8Q2HV+83 New York
Nearby Locations:
Carnegie Hill | Yorkville | Lenox Hill | Upper East Side | Midtown Manhattan
10029 | 10028 | 10021| 10044, 10065, 10075, 10128 | 10022
Working Hours:
Monday: 9AM-6PM
Tuesday: 9AM-6PM
Wednesday: 9AM-6PM
Thursday: 9AM-6PM
Friday: 9AM-4PM
Saturday: Closed
Sunday: Closed
Payment: cash, check, credit cards.
Directory:
Tags:

Dental Cleanings or Prophylaxis (“prophy”) is an essential component of preventive dentistry. The goal is to remove microbial plaque which can cause gingivitis (gum inflammation), and cavities.
Only our professional staff can determine how frequently this must be done. Some patients accumulate tartar faster than others.
Prophylaxis and Why It Will Help Your Kid
If you regularly visit a pediatric dentist then it’s likely you have your teeth professionally cleaned at least twice a year. This is to remove any hardened plaque or tartar from teeth which helps keep your teeth and gums in great shape.
Prophylaxis reduces the risk of gum disease and tooth decay and your kid needs regular professional dental cleanings for exactly the same reasons as you. During this appointment, it’s also possible for the hygienist to identify any areas your child might be missing whenever they brush or floss their teeth.
This will allow your local kid’s dentist to provide personalized oral hygiene instructions to help your child brush in the most effective way possible. If they do need any tuition on how to brush and floss then you can be sure it will be done in a way that is entertaining and fun.
Read more: https://www.nycpediatricdentist.com/dental-cleaning/
Pediatric Dentistry: Dr. Sara B. Babich, DDS
116 E 84th St,
New York, NY 10028
(212) 988–4070
Web Address:
https://www.nycpediatricdentist.com/
Our location on the map: https://g.page/dr-sara-babich-pediatric-dds-nyc
https://plus.codes/87G8Q2HV+83 New York
Nearby Locations:
Carnegie Hill | Yorkville | Lenox Hill | Upper East Side | Midtown Manhattan
10029 | 10028 | 10021| 10044, 10065, 10075, 10128 | 10022
Working Hours:
Monday: 9AM-6PM
Tuesday: 9AM-6PM
Wednesday: 9AM-6PM
Thursday: 9AM-6PM
Friday: 9AM-4PM
Saturday: Closed
Sunday: Closed
Payment: cash, check, credit cards.
Directory:
Tags:

Silver Diamine Fluoride, SDF, is an alternative treatment for tooth decay under certain conditions. Treatment of children’s deciduous (primary or “baby”) and permanent (“adult”) teeth with silver diamine fluoride is a rather new strategy provided by pediatric dentist Dr. Babich located on Manhattan’s Upper East Side aimed at preventing tooth decay (dental caries) and at arresting existing tooth decay.
What Is Tooth Decay?
Tooth decay is a bacterial infection, in which bacteria of the oral cavity, the main culprit is Streptococcus mutans, metabolize dietary sugars to sticky polymers that allow them to adhere within a biofilm to the tooth surface. In addition, bacterial metabolism of dietary sugars forms acidic end-products that demineralize (i.e., soften) the enamel, the hard tooth’s outer surface.
If left unchecked, the bacterial infection will advance, burrowing deeper into the tooth structure, first into the dentin, and thereafter to the pulp, which houses nerve endings and blood vessels. Recognizing that tooth decay is a bacterial disease, the strategy behind the topical application of silver diamine fluoride to tooth surfaces is to inhibit bacterial growth in existing areas of decay and to prevent the occurrence of areas of new decay.
Read more: https://www.nycpediatricdentist.com/silver-diamine-fluoride-treatment/
Pediatric Dentistry: Dr. Sara B. Babich, DDS
116 E 84th St,
New York, NY 10028
(212) 988–4070
Web Address:
https://www.nycpediatricdentist.com/
Our location on the map: https://g.page/dr-sara-babich-pediatric-dds-nyc
https://plus.codes/87G8Q2HV+83 New York
Nearby Locations:
Carnegie Hill | Yorkville | Lenox Hill | Upper East Side | Midtown Manhattan
10029 | 10028 | 10021| 10044, 10065, 10075, 10128 | 10022
Working Hours:
Monday: 9AM-6PM
Tuesday: 9AM-6PM
Wednesday: 9AM-6PM
Thursday: 9AM-6PM
Friday: 9AM-4PM
Saturday: Closed
Sunday: Closed
Payment: cash, check, credit cards.
Directory:
Tags:

SAVE 20% ON YOUR FIRST EXAM
Precision Dental NYC is always accepting new patients! Save 20% on first exam, which includes X-rays and a cleaning. Be sure to mention this offer when you schedule your exam.
Precision Dental NYC
21–34 30th Ave,
Queens, NY 11102
(718) 274–2749
Web Address: https://precisiondentalnyc.com
Our location on the map: https://g.page/Precision-Dental-NYC
https://plus.codes/87G8Q39F+M8 Astoria
Nearby Locations:
Astoria | Ditmars Steinway | Astoria Heights | Jackson Heights | Woodside | Sunnyside Gardens | Dutch Kills
11101, 11102, 11103, 11104, 11105, 11106 | 11372 | 11377
Working Hours:
Monday: 9AM-7PM
Tuesday: 9AM-7PM
Wednesday: Closed
Thursday: 9AM-7PM
Friday: Closed
Saturday: 9AM-4PM
Sunday: Closed
Payment: cash, check, credit cards.
Directory:
Tags:

SAVE 20% ON DENTAL IMPLANT PROCEDURES
If you’re missing teeth and are concerned about being able to afford a solution, Precision Dental NYC is here for you! With 20% savings on any Dental Implant procedures, you can have a beautiful smile in no time. We’re here to help our Chicago neighbors get the smile they deserve for a price they can afford! Don’t put off your dream smile any longer. Schedule your appointment today to take advantage of this offer.
Precision Dental NYC
21–34 30th Ave,
Queens, NY 11102
(718) 274–2749
Web Address:
https://precisiondentalnyc.com
Our location on the map:
https://g.page/Precision-Dental-NYC
https://plus.codes/87G8Q39F+M8 Astoria
Nearby Locations:
Astoria | Ditmars Steinway | Astoria Heights | Jackson Heights | Woodside | Sunnyside Gardens | Dutch Kills
11101, 11102, 11103, 11104, 11105, 11106 | 11372 | 11377
Working Hours:
Monday: 9AM-7PM
Tuesday: 9AM-7PM
Wednesday: Closed
Thursday: 9AM-7PM
Friday: Closed
Saturday: 9AM-4PM
Sunday: Closed
Payment: cash, check, credit cards.
Directory:
Tags:
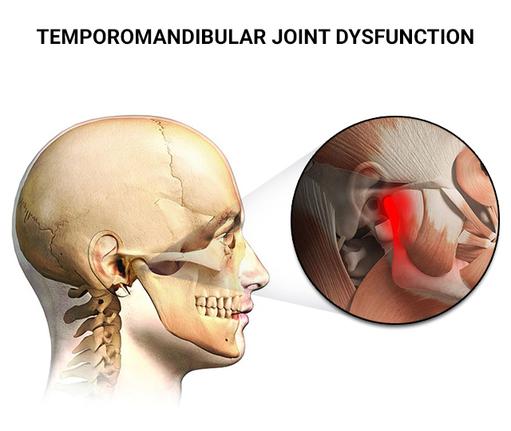
Temporomandibular Joint Dysfunction Syndrome (TMJ) is a common condition affecting a wide variety of people. TMJ is characterized by severe headaches, jaw pain of varying degrees, grinding teeth, and an intermittent ringing in the ears. The vast majority of TMJ sufferers are unaware that the root cause of these problems is something that a dentist can effectively treat. The symptoms of TMJ are debilitating and can greatly interfere with everyday life. The comfort and general well being of the patient are at the heart of the dental practice, so pain relief is the first consideration of the dentist. Our dental team are able to test, diagnose, and devise an immediate plan to treat the underlying causes of the TMJ disorder.
What Causes Jaw Pain?
The most common cause of jaw pain is due to an injury or abnormality affecting the joint hinging your jaw, called the temporomandibular joint. It’s a problem called a temporomandibular joint disorder or TMD or TMJ and is estimated to affect nearly 10 million people in the United States alone.
Several different things can cause TMJ as it can be due to the muscles controlling jaw movement becoming painful, or because of injury to the jaw joint. Excessively stimulating the jaw joint can cause jaw pain, and sometimes the disc that helps to cushion jaw movements becomes displaced or damaged. This disc can also become affected by arthritis.
Read more: https://precisiondentalnyc.com/tmj-temporomandibular-joint-dysfunction/
Precision Dental NYC
21–34 30th Ave,
Queens, NY 11102
(718) 274–2749
Web Address: https://precisiondentalnyc.com
Our location on the map: https://g.page/Precision-Dental-NYC
https://plus.codes/87G8Q39F+M8 Astoria
Nearby Locations:
Astoria | Ditmars Steinway | Astoria Heights | Jackson Heights | Woodside | Sunnyside Gardens | Dutch Kills
11101, 11102, 11103, 11104, 11105, 11106 | 11372 | 11377
Working Hours:
Monday: 9AM-7PM
Tuesday: 9AM-7PM
Wednesday: Closed
Thursday: 9AM-7PM
Friday: Closed
Saturday: 9AM-4PM
Sunday: Closed
Payment: cash, check, credit cards.
Directory:
Tags:
What’s Considered a Dental Emergency?
If you knock a tooth out, you know immediately that you need urgent dental care. But an emergency isn’t always so cut-and-dried. If you don’t feel much pain, maybe you can wait a few days to visit your dentist. But if you experience more severe tooth pain or pain in your gums or jaw, don’t hesitate to call your dentist.
You can exacerbate your problems by waiting. Dental issues rarely go away on their own. You need the best dental care. Symptoms and conditions that constitute an immediate dental emergency include:
- Bleeding from your mouth. If your gums or inner cheeks are bleeding and won’t stop, that’s a condition that requires 24-hour emergency dental care or a trip to the nearest emergency room. Try to stop the bleeding, but you need urgent dental care to ease the swelling and pain.
- A broken tooth. If a tooth has been knocked out entirely or a piece has broken off, you definitely need emergency dental care. Find the tooth that fell out, put it in saline or milk, and get to your dentist or emergency room. If you don’t act quickly, you may lose the tooth forever.
- A loose or detached crown or filling. If a filling or crown falls out or even becomes loose, you feel the pain immediately, since now your tooth pulp is unprotected and exposed. Even a breath can cause pain. You may have a metallic taste. Get to an emergency dental facility for treatment. Otherwise, you may need a root canal.
- Nerve pain. Pain from an exposed nerve in your tooth is intense. It’s constant and may even be throbbing. You need urgent dental care to save the tooth. If the pain suddenly disappears, that’s a sign the tooth nerves are dead or dying.
- Any swelling around your mouth. Inflammation signals a problem. You won’t know why your mouth is swelling until you get in to see your dentist, who can examine you with an experienced eye. It may be an abscessed tooth or something even more severe.
- A tooth with an abscess. An abscess is an infection beneath your tooth. It can cause difficulty in breathing, eating, and drinking. Since infections can attack nearby teeth, seek immediate emergency dental care.
- Severe tooth decay. If the cavity is left untreated, it can damage the tooth pulp without the possibility of restoration. When tooth decay is beyond what can be treated with a root canal or dental fillings, emergency tooth extraction will be required.
- Some food stuck in your mouth. Bits of popcorn, shells, or candy can get stuck between your teeth or between your teeth and gums. It can irritate your gums, causing pain and swelling. If you can’t reach it, see your dentist for emergency toothache relief.
- Pain without a known cause. When you’re feeling acute or dull pain, and you don’t know the cause of the pain, you need urgent dental care. Pain always signals a health issue, and if you don’t know the reason, your dentist has to make a diagnosis before it can be treated.
Precision Dental NYC
21–34 30th Ave,
Queens, NY 11102
(718) 274–2749
Web Address: https://precisiondentalnyc.com/
Our location on the map: https://g.page/Precision-Dental-NYC
https://plus.codes/87G8Q39F+M8 Astoria
Nearby Locations:
Astoria | Ditmars Steinway | Astoria Heights | Jackson Heights | Woodside | Sunnyside Gardens | Dutch Kills
11101, 11102, 11103, 11104, 11105, 11106 | 11372 | 11377
Working Hours:
Monday: 9AM-7PM
Tuesday: 9AM-7PM
Wednesday: Closed
Thursday: 9AM-7PM
Friday: Closed
Saturday: 9AM-4PM
Sunday: Closed
Payment: cash, check, credit cards.
Directory:
Tags:

Born in Russia, Dr. Alexander Bokser immigrated to the United States at the age of ten. Settling in Kew Gardens Queens, Dr. Bokser graduated from Queens College with a B.A. in Economics. He then received his degree at New York University College of Dentistry in 1994, where he was licensed by the New York State Board of Regents, and the North East Regional Board of Dental Examiners.
Dr. Bokser completed his residency at Flushing Hospital, which was associated with Albert Einstein School of Medicine in 1995. Afterwards, he was asked to join the Hospital as an attending, where he has been teaching ever since, assuming the role of educator and mentor.
Dr. Bokser has been in private practice since 1996 in Astoria, Queens. Dr. Irene Bokser, Diplomate of the American Board of Periodontology, joined the practice in 2009. She maintains her own practice in Bayside, Queens. The focus of their practice is on oral rehabilitation, implants, cosmetic dentistry, periodontics, and general dentistry.
Dr. Alexander Bokser has received numerous awards in dentistry and community service, and is a member of the American Dental Association, Academy of General Dentistry, and North Queens Dental Study Club.
Dr. Bokser resides in Long Island, NY with his wife, Dr. Irene Bokser, and two children. He enjoys photography, outdoors and travel, and most of all, spending time with his family.
Precision Dental NYC
21–34 30th Ave,
Queens, NY 11102
(718) 274–2749
Web Address:
https://precisiondentalnyc.com
Our location on the map:
https://g.page/Precision-Dental-NYC
https://plus.codes/87G8Q39F+M8 Astoria
Nearby Locations:
Astoria | Ditmars Steinway | Astoria Heights | Jackson Heights | Woodside | Sunnyside Gardens | Dutch Kills
11101, 11102, 11103, 11104, 11105, 11106 | 11372 | 11377
Working Hours:
Monday: 9AM-7PM
Tuesday: 9AM-7PM
Wednesday: Closed
Thursday: 9AM-7PM
Friday: Closed
Saturday: 9AM-4PM
Sunday: Closed
Payment: cash, check, credit cards.
Find us at: https://doctor.webmd.com/doctor/alexander-bokser-D9247052-2B75-41EB-8C9D-A85EE352D85B-overview
Directory:
Tags:

Do you feel your teeth are a little shorter than you’d like, or your smile appears “gummy”? Our dental provider can give you a wider, more symmetrical smile through a crown lengthening procedure. The dentist removes excess gum or bone tissue during this treatment, reveals more of your natural tooth, and creates a more even gum line.
You may also need crown lengthening if you require a restorative dental procedure, such as fixing a broken tooth or getting a porcelain crown. If you have any questions about crown lengthening or if you’d like Dr. Bokser to review your options, contact our dental center today to schedule an appointment.
What is a Crown Lengthening Procedure?
Crown Lengthening Mouth Only
Crown lengthening is a common surgical procedure performed by Dr. Bokser, who will extend the height or size of the portion of the tooth that is visible above the gum line.
Crown lengthening in Astoria is typically performed to improve the health of the gum tissue or prepare your mouth for certain restorative procedures – for example, if not enough of the tooth sticks out above the gum line to support a filling or crown. You may also consider crown lengthening if your smile can be described as “gummy,” where the teeth are covered with excess gum tissue.
Crown lengthening is a common surgical procedure performed by Dr. Bokser, who will extend the height or size of the portion of the tooth that is visible above the gum line. The doctor will typically use local anesthesia and then gradually reshape or remove the excess gum and bone tissue to expose the natural tooth.
Precision Dental NYC
21–34 30th Ave,
Queens, NY 11102
(718) 274–2749
Web Address: https://precisiondentalnyc.com
Our location on the map: https://g.page/Precision-Dental-NYC
https://plus.codes/87G8Q39F+M8 Astoria
Nearby Locations:
Astoria | Ditmars Steinway | Astoria Heights | Jackson Heights | Woodside | Sunnyside Gardens | Dutch Kills
11101, 11102, 11103, 11104, 11105, 11106 | 11372 | 11377
Working Hours:
Monday: 9AM-7PM
Tuesday: 9AM-7PM
Wednesday: Closed
Thursday: 9AM-7PM
Friday: Closed
Saturday: 9AM-4PM
Sunday: Closed
Payment: cash, check, credit cards.






