Tag
Directory:
Tags:
- Hydrocephalus is a chronic condition that occurs when excess cerebrospinal fluid (CSF) collects in your brain’s ventricles and increases pressure inside your head
- Failure to treat the condition can lead to morbidity and death
- First line therapy is the surgical insertion of a ventriculoperitoneal shunt (VPS) to restore your CSF circulation
- A significant risk with the procedure is infection
- To reduce infection manufacturers’ impregnate standard shunts with either silver or antibiotics and market the impregnated shunts at higher prices
- Which VPS (standard, silver or antibiotic) provides patients with the most protection from infection?
- Which VPS is most cost effective for healthcare systems?
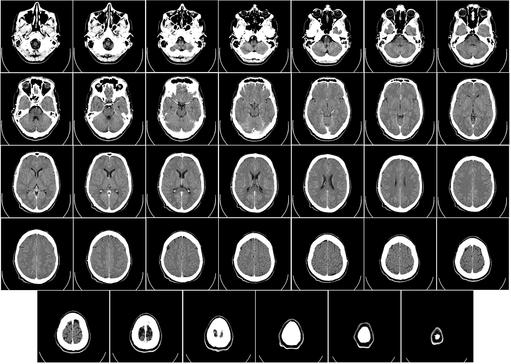
“It” is Hydrocephalus; a chronic condition that occurs when excess cerebrospinal fluid (CSF) collects in your brain’s ventricles, (fluid-filled areas). CSF disperses from your ventricles around your brain and spinal cord. Too much CSF may result in an accumulation of fluid, which can cause the pressure inside of your head to increase. In a child, this causes the bones of an immature skull to expand and separate to a larger-than-normal appearance.
There are no medical therapies to effectively treat hydrocephalus. The only viable treatment is surgical. The gold standard therapy is the insertion of a ventriculoperitoneal shunt (VPS), which is a common surgical procedure to restore your CSF circulation, regulate its flow and allow you to have a normal daily life. Notwithstanding, a significant challenge is infection at the site of the surgical wound, the shunt or in the cerebrospinal fluid itself (meningitis). This effects about 15% of hydrocephalus patients and may result in further surgeries, extended hospital stays, a reduction in your quality of life and a significant hike in healthcare costs.
To reduce potential infection manufacturers’ impregnate standard shunts with either silver (silver has benefits in reducing or preventing infection) or antibiotics and market the impregnated shunts at higher prices.
There are two principal classifications for hydrocephalus: (i) communicating and (ii) non-communicating hydrocephali. Both can be subdivided into congenital (present at birth) and acquired (occurs following birth). Communicating hydrocephalus can also be subdivided into normal pressure hydrocephalus (NPH) and hydrocephalus ex-vacuo, which occurs when there is damage to your brain caused by stroke or injury. It is generally understood that congenital hydrocephalus can be caused by genetic defects, which can be passed from one or both parents to a child, but the direct hereditary links are still being investigated. Notwithstanding, experts have found a connection between a rare genetic disorder called L1 syndrome and hydrocephalus. L1 syndrome is a group of conditions that mainly affects the nervous system and occurs almost exclusively in males.
Most babies born with hydrocephalus or who develop hydrocephalus as infants will have a normal lifespan, and approximately 40 to 50% will have normal intelligence. Seizure disorders have been diagnosed in about 10% of children with hydrocephalus and the mortality rate for infants is approximately 5%.
In the video below Sanj Bassi, a Consultant Neurosurgeon at King’s College Hospital, London and a member of the London Neurosurgery Partnership, describes hydrocephalus:

Causes
Signs and symptoms
Diagnosing hydrocephalus
In the video below Bassi describes how hydrocephalus is diagnosed:
A shunt consists of two thin, long flexible hollow tubes, called catheters, with a valve that keeps fluid from your brain flowing in the right direction and at the proper rate and thereby reduces brain pressure to a safe level. To install a shunt a surgeon will make a small insertion behind your ear and also drill a small borehole in your scull. One catheter is then threaded into one of your brain’s ventricles through the hole in your scull, and the other is inserted behind your ear and threaded subcutaneously down to your chest and into your abdomen where excess CSF can drain safely, and your body can reabsorb it. Your surgeon may attach a tiny pump to both catheters and place it under the skin behind your ear. The pump will automatically activate to remove fluid when the pressure in your skull increases. Shunts can be programmable (externally adjustable by a magnetic device) to activate when the fluid increases to a certain volume, or non-programmable. Most surgeons tend to choose a programmable model, despite the fact that in clinical studies both types perform comparably.
To determine the relative clinical benefits and cost-effectiveness of the three different ventriculoperitoneal shunts (standard, silver or antibiotic) following their de novo insertions, the UK’s National Institute for Health Research funded a large prospective multi-centre randomised controlled clinical study - The British Antibiotic and Silver Impregnated Catheters for Ventriculoperitoneal Shunts Study - (BASICS). Findings were published in the September 2019 edition of The Lancet. These concluded that shunts impregnated with antibiotics significantly reduce the risk of infection and also healthcare costs compared to both standard shunts and those impregnated with silver. Conor Mallucci, Consultant Paediatric Neurosurgeon at Alder Hey Children’s Hospital, Liverpool, UK, and lead author of the study, suggests that shunts impregnated with antibiotics should be, “the first choice for patients with hydrocephalus undergoing insertion of their first ventriculoperitoneal shunt”.
All shunts used in the study were CE marked medical devices intended for the condition. Participants were randomly assigned to three groups: one group of 536 received a standard shunt, another of 531 received a silver impregnated shunt, and a third group of 538 received an antibiotic impregnated shunt. The minimum patient follow-up period was six months and the maximum two years. Six per cent of evaluable patients in both the standard and silver groups presented with infections and required a shunt revision. This compared to only 2% in the antibiotic impregnated shunt group that became infected and needed revising. The difference is significant.
The Study’s economic findings
The research has a further significance because, despite the high medical costs of treating hydrocephalus, the annual spend on hydrocephalus research is relatively low. For example, the US National Institutes of Health (NIH) invests less than US$8m per year in hydrocephalus research. This means that there is a dearth of clinical studies associated with the condition and no long-term follow-up research over the lifetime of patients.
Although BASICS is a significant study it should be mentioned that it is restricted by the relatively low proportion of patient-reported outcomes: 32, 31 and 12 reported infections after insertion of the standard, silver and antibiotic VPS’s respectively.
Takeaways









