Search results
Directory:
Tags:

- Diabetic foot ulcers (DFUs) are a result of diabetes complications and can lead to amputations and death
- Scientists and clinicians struggle to reduce the vast and escalating burden of DFUs
- In wealthy countries like the UK there are specialist multidisciplinary diabetic foot clinics
- New and innovative therapies are beginning to emerge, which accelerates the rate of complete wound closure for DFUs
- Notwithstanding new products coming to market, the best therapy is prevention
This Commentary discusses diabetic foot ulcers (DFUs) within the context of chronic wounds. Although chronic wounds tend to be an overlooked area of medicine and do not feature prominently in the popular media; NHS England, spends £5bn a year treating 2m patients with chronic wounds. The incidence rates of people affected with wounds are rising fast and some experts suggest that nearly 60% of all wounds become chronic. According to Una Adderley, a wound expert and Director of NHS England’s National Wound Care Strategy Programme, therapy in England for chronic wounds is patchy and suboptimal, “leading to non-healing or delayed healing (which) increases the number of people living with chronic wounds. Too many people are receiving care for which there is little evidence that it works and too few are receiving care for which there is strong evidence that it works”.
According to a 2019 report by the consulting firm MarketsandMarkets the global wound care market in 2019 is estimated to be US$20bn and projected to reach US$25bn by 2024. Market drivers include the vast and fast-growing incidence rates of hard-to-heal chronic wounds, a large proportion of which are associated with diabetes, increasing R&D spending, technological developments, the growing use of regenerative medicine in wound care, recent advances in molecular data that have contributed to genome sequencing, and the increasing use of AI in the management of wound care solutions. The chronic wound care markets of North America and Europe are expected to grow at a CAGR of ~4.5% for the next 5 years, but the highest CAGR is expected in Asia where the vast pool of patients is increasing significantly, and favourable reimbursement policies are expected to persist in the region for the next decade.
When accompanied by an underlying condition such as diabetes, chronic wounds in the form of DFUs, are challenging to heal and have a deleterious effect on your quality of life: you experience pain, suffering, disfigurement, anxiety impaired mobility, malodour and social isolation. Because the prevalence of diabetes is increasing worldwide, DFUs have become a large, severe and growing public health issue as described in two research papers published in 2019.
One, published in the May 2019 edition of Diabetic Medicine, reports findings of an 18 year study of DFUs, and suggests that although current therapies in the UK result in better than previously reported survival in persons < 65 years (10 year survival is 85%), treatments fail to, “reduce recurrent incidence (of DFUs and) cumulative prevalence of all ulcers continues to increase”; from 20.7 to 33.1 per 1,000 persons between 2003 to 2017. The second paper, published in the January-March 2019 edition of the International Journal of Applied Basic Research, report sfindings of a prospective Indian study of 63 patients >18 with DFUs and shows the increase in the severity of DFUs and the consequent increase in the rate of hospital readmissions, amputations and mortality.
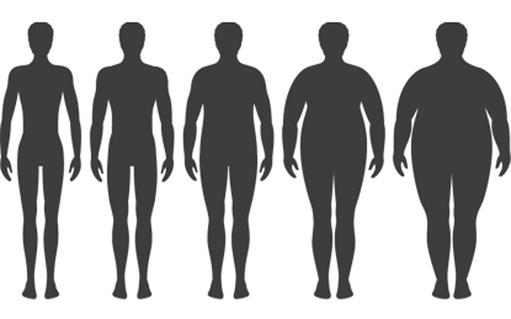
Diabetes is a chronic disease that occurs either when your pancreas does not produce enough insulin or when your body cannot effectively use the insulin it produces. Insulin is a hormone that regulates your blood sugar level. High blood sugar levels (hyperglycaemia) is a common effect of uncontrolled diabetes and can lead to serious complications, which include blindness, kidney failure, heart attacks, stroke, diabetic foot ulcers (DFUs), and lower limb amputations. According to the World Health Organization, the global prevalence of diabetes among people >18 has risen from 4.7% in 1980 to 8.5% in 2014. Today, some 422m people worldwide have diabetes, which has increased from 108m in 1980. There is expected to be some 642m people >18 living with diabetes by 2040.
If you have diabetes you are prone to ulcers because your increased blood sugar levels create thick, sticky blood, which can lead to peripheral artery disease (PAD), neuropathy (a loss of sensation due to nerve damage), and/or problems with circulation due to damage to your small blood vessels, which reduce your body’s ability to heal injuries.
Signs and symptoms of DFUs include numbness in your toes and a loss of feeling in your feet, painful tingling sensations, blisters, minor abrasions and cuts without pain that do not heal, skin discoloration and temperature changes With a loss of sensation, a minor injury to your foot can go unnoticed and untreated, and quickly lead to an ulcer. If you are living with diabetes, ulceration is an ongoing challenge. Only about 66% of DFUs eventually heal without surgery. If you have had a foot ulcer you are at increased risk of further ulceration. Studies suggest that around 25% of people living with diabetes who become ulcer-free have developed new ulcers within 3 months, and 34% to 41% within 12 months. Some foot ulcers are painful, and treatment often requires that you spend a significant amount of time visiting clinics to frequently change your wound dressings. The poor prognosis of DFUs is often attributed to other complications of diabetes such as peripheral neuropathy, peripheral vascular disease and persistent hyperglycaemia. Managing diabetic foot ulcers is a major challenge for healthcare systems globally and the main cause of more than half of nontraumatic lower limb amputations: every 30 seconds in the world, a lower limb is amputated due to diabetes. Amputations have life-altering repercussions for patients and represent a significant burden for the healthcare industry as a whole. Between 0.03% and 1.5% of people with DFUs require an amputation and most amputations start with ulcers.
For major amputations, the prognosis is poor because your other limb is at risk. Research suggests that only around 50% of patients survive for two years after major diabetes related amputations. The one-year mortality rate has been estimated at 32.7% after major amputation and 18.3% after minor amputation if you have diabetes. Five-year cumulative mortality for patients with diabetes undergoing a first major amputation has been estimated at 68% to 78.7%. Thus, if you have diabetes and a DFU you have almost a 50% chance of being dead within five years, which is significantly higher than for people with either breast (18%) or prostate (8%) cancers.
In the UK some 70,000 to 90,000 people living with diabetes have DFUs at any one time. If you have diabetes you are about 23 times more likely to experience an amputation than someone without diabetes. In England, diabetes leads to more than 9,000 lower limb amputations each year. Each week in England some 169 people undergo an amputation procedure as a result of diabetes. Analysis by the charity Diabetes UK found that between 2014 and 2017, 26,378 people had lower limb amputations linked to diabetes, which represented a 19% rise from 2010 to 2013. Diabetes affects almost 3.7m people in the UK. In 2017 NHS England launched a special transformation fund aimed at improving patients with diabetes access to specialist multidiscipline foot care clinics to help avoid amputations.
In the video below Hisham Rashid, Consultant Vascular Surgeon at King’s College Hospital, London, describes a DFU and explains why they benefit from specialist multidisciplinary treatment centres. “DFUs have similar features to other ulcers, and often present in the toes and heal areas of the foot with the loss of skin and an exposed base with infection and necrosis. The significant difference is that a DFU usually comes with multiple pathologies, which, in addition to infection, include neuropathy and peripheral vascular disease. DFUs do not heal quickly and often require vascular surgeons working closely with radiologists, orthopaedic surgeons to correct any deformity and a microbiology unit to manage infection,” says Rashid.
Rashid also explains that different therapies are used to heal DFUs. “If the patient has peripheral artery disease (ischaemia) then this has to be treated first with an angioplasty or a bypass or both to improve blood circulation into the foot. Once this is achieved, the ulcer is debrided and dressed. There are different dressings, which include negative pressure dressing, which sucks the blood into the tissues and thereby promotes healing. Sometimes skin graphs are necessary to get the tissue to heal faster. This can be done as a day surgery using local anaesthetic,” says Rashid.
Prevention of DFUs
Given the severity of DFUs and their vast and rapidly increasing burden on individuals with diabetes and healthcare systems, increasing attention is being devoted to prevention, which involves adequate glycaemic control and modification of risk factors. While education is an obligation of healthcare professionals, it is crucial that people living with diabetes themselves increase their awareness and understanding of the condition and integrate regular feet examination and care into their daily lives. In the video below, Roni Sharvanu Saha, Consultant in Acute Medicine, Diabetes and Endocrinology, St George’s Hospital, London, suggests that, “We’re getting better at understanding why DFUs occur, and better at examining peoples’ feet. In England, if you have diabetes you are entitled to a clinical examination of your feet at least twice a year. Checks include whether you have any minor abrasions, or whether you can distinguish hot and cold water with your feet, and signs that you might have problems with your circulation and nervous system. Ensuring that people living with diabetes receive regular checks means that if you have reduced or poor circulation, you’re referred to the correct specialty team in order to protect you from developing DFUs. Prevention is better that cure. If we can get better at examining feet, outcomes will improve. If diabetes is not controlled complications will occur”.
With the well-being of millions of people living with diabetes at stake, there is a pressing need for therapies that bring DFUs to closure as quickly as possible. The current standard of care (SOC) regimen for DFUs involves maintaining a moist wound environment, debriding nonviable tissue, relieving pressure with an offloading boot and preventing or managing wound infection. Even with a good SOC, DFUs are notoriously slow to close, creating a demand for new and innovative medicines and techniques to enhance closure. Increasingly, there are advanced therapies to facilitate healing DFUs when traditional approaches fail.
An example of a relatively new product to help close DFUs is human amniotic membrane. Amniotic membrane has been used for wound healing purposes since the early 20th century, but it represents a relatively recent and promising advanced therapy to accelerate healing in DFUs. Amniotic membrane is derived from the human placental sac that supports the foetus by forming the inner lining of the amniotic cavity. Functions of amniotic membrane include the exchange of water-soluble molecules and the production of cytokines and growth factors to facilitate the development of the foetes. The anatomic makeup of amniotic membrane dictates its functionality, and a significant characteristic is its ability to produce a wide variety of regenerative growth factors that facilitate foetal development. These growth factors, in combination with various other cytokines, have substantial potential benefits in wound healing, which include creating a structural scaffold for tissue proliferation, modulating the immune response, reducing inflammation, stimulating angiogenesis and facilitating tissue re-modelling.
Two small but significant prospective cohort studies on the effectiveness of human amniotic tissue to treat DFUs were reported in the journal Wounds. One in the March 2016 edition and another in the November 2017 edition. The first is a prospective, randomized, multicentre, controlled study and the second a retrospective cohort study of 20 patients. In both studies amniotic membrane is used in combination with SOC, including debridement, well-controlled offloading, management of bacterial burden, and adequate perfusion.
Both studies suggested that the use of amniotic membrane is more likely to: (i) lead to complete wound closure, (ii) accelerate the rate of wound closure, and (iii) present no additional safety risks when compared to SOC alone in the treatment of DFUs. The first study demonstrated a statistically significant advantage of an amniotic membrane as compared to SOC in facilitating closure of chronic DFUs. 45% of participants achieved complete wound closure, while 0% of SOC participants alone achieved complete wound closure within 6 weeks. Further, there appears to be no increased rate of adverse events associated with the use of amniotic membrane in these wounds. The second study was a retrospective cohort study using a human amniotic membrane on 20 patients presenting with DFUs and venous leg ulcers. Patients underwent a 2-week ‘run-in’ period with good SOC; and if upon their return the ulcer had closed ≥ 30% in area, the subject was excluded from participation in the study. All wounds were effectively closed in approximately 10 weeks, DFUs in 12 weeks and venous leg ulcers in 9 weeks, and no adverse events were noted, suggesting that the therapy using human amniotic membrane is safe.
The most significant limitation of both studies is their small sample size, which decreases the generalizability of their findings. Notwithstanding, the studies suggest that amniotic tissue products are efficacious options for DFUs when used in conjunction with the current SOC, which includes aggressive sharp debridement, adequate offloading and the application of sterile dressings. Further, amniotic membrane, like most biologic tissue products, requires significant processing and therefore its cost is relatively high: on average between US$500 to US$1,000 per application. Notwithstanding, these costs are significantly less than the average annual therapy cost of US$28,000 per patient for SOC for a DFU. And therefore, using amniotic tissue in the therapy for DFUs could result in significant savings for healthcare systems. Tissue storage as well as the time and skill required to apply amniotic membranes also represent challenges inherent to these products.
Millions of people are living with diabetes, which, if not managed appropriately can lead to life-changing complications. A DFU is one such complication, which often starts with a minor abrasion on your ankle or toe that you do not feel and therefore tend not to perceive to be important, until that is, it quickly escalates into a chronic wound that does not heal and eventually leads to a lower limb amputation. In most wealthy nations, health providers are aware of the dangers of DFUs and have set up multi-disciplinary diabetic foot clinics to treat and manage the condition. However, access to such clinics is patchy and the prevalence of DFUs continues to increase, and the eye-watering costs of treating and managing DFUs continue to escalate. In recent years, the therapy for DFUs has been improved by technological advances. We describe one of these: the use of amniotic tissue in conjunction with standard of care protocols. Recent research findings suggest that the use of amniotic tissue holds out the possibility not only of significant therapeutic benefits, but also of substantial cost savings for healthcare systems. Notwithstanding, perhaps the most efficacious therapy for DFUs is prevention. This means investing in effective education and awareness programs, good glycaemic control and appropriate footwear; encouraging people living with diabetes to participate in regular foot examinations and screening for peripheral neuropathy and peripheral arterial disease, and insisting that early telltale signs of foot wounds, no matter how minor, should be immediately referred to a specialist clinic.

During these unprecedented challenging times caused by the coronavirus CoVID-19 pandemic, we trust that you all stay safe and well and let the spirit of Ramadan remain in your hearts and light up your souls from within.
Directory:
Tags:

|
Directory:
Tags:

|
Directory:
Tags:
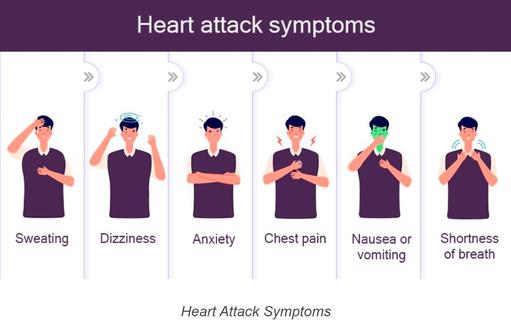
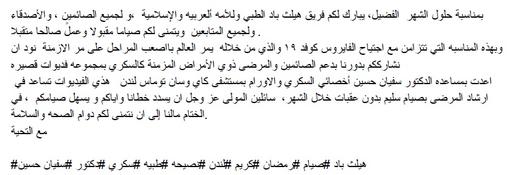
The leading killers in the United States are heart attacks and strokes. Annually, around 860,000 Americans die from heart disease or another untreated cardiovascular condition. The most preventable precursors to a heart attack are high blood pressure, bad nutrition habits, high cholesterol, smoking, limited or no physical exercise, obesity and type 2 diabetes.
Heart attacks and strokes are the leading causes of death in the United States. Every year, around 860,000 Americans die as a result of heart disease or another untreated cardiovascular condition. High blood pressure, poor nutrition, high cholesterol, smoking, little or
best cardiovascular specialist in NYC no physical activity, obesity, and type 2 diabetes are the most preventable precursors to a heart attack.
The onset of a heart attack can be sudden and severe, but most begin as a gradually increasing pain in your chest. In the United States, a heart attack occurs about once every 40 seconds. Strenuous activities like sports, heavy labor, and other physical activities are often credited as an inciting cause of a heart attack. But the real causes are typically longstanding health issues that are varied and complex.
Read more: https://newyorkcardiac.com/heart-attack
New York Cardiac Diagnostic Center
115 East 86th Street
New York, NY 10028
(212) 860–0796
Web Address: https://newyorkcardiac.com/
Our locations on the map:
https://g.page/Cardiologist-Upper-East-Side-NYC
https://plus.codes/87G8Q2JV+2G New York
Nearby Locations:
Upper East Side
Yorkville | Manhattan | Lenox Hill | Carnegie Hill | East Harlem
10028, 10075, 10128 | 10021 | 10029 | 10035
New York Cardiac Diagnostic Center
200 West 57th Street, Suite 200
New York, NY 10019
(212) 582–8006
Our locations on the map:
https://g.page/New-York-Cardiology-Midtown-NYC
https://plus.codes/87G8Q289+5Q New York
Nearby Locations:
Midtown
Hell`s Kitchen | Little Brazil | Lenox Hill | Diamond District
10019 | 10036 | 10021 | 10017
New York Cardiac Diagnostic Center
65 Broadway Suite 1806
New York, NY 10006
(212) 860–5404
Our locations on the map:
https://g.page/New-York-Cardiology-Downtown-NYC
https://plus.codes/87G7PX4Q+W2 New York
Nearby Locations:
Financial District / Wall Street
World Trade Center | Two Bridges | Tribeca | Lower East Side
10007 | 10002 | 10003, 10009
Working Hours:
Monday: 8 am — 5 pm
Tuesday: 8 am — 5 pm
Wednesday: 8 am — 5 pm
Thursday: 8 am — 5 pm
Friday: 8 am — 5 pm
Saturday: Closed
Sunday: Closed
Payment: cash, check, credit cards.
In today’s digital health era, Software as a Medical Device (SaMD) is transforming how healthcare providers deliver patient care. Unlike traditional medical devices, SaMD refers to software that performs medical functions on its own—without being part of a physical device. Examples include mobile apps that monitor heart rhythms, AI-based imaging tools, and platforms that support chronic disease management.
Why Is SaMD Important?
SaMD plays a crucial role in enhancing accessibility, efficiency, and accuracy in healthcare. By leveraging algorithms, data analytics, and cloud-based solutions, it allows clinicians to make real-time, informed decisions. For patients, SaMD provides the benefit of remote monitoring and personalized care, especially in areas like mental health, diabetes management, and cardiovascular health.
Key Benefits of SaMD
1. Improved Diagnostics – AI-driven software can detect conditions earlier and more accurately.
2. Remote Care – Enables monitoring outside traditional hospital settings.
3. Cost Efficiency – Reduces the need for frequent in-person visits.
4. Scalability – Cloud-based SaMD can be deployed across multiple healthcare systems with ease.
Future Outlook
The adoption of Software as a Medical Device (SaMD) is set to grow as healthcare systems embrace digital transformation. With advancements in AI, machine learning, and regulatory support from bodies like the FDA, SaMD is becoming an essential pillar of modern healthcare delivery.
Directory:
Tags:

|
Directory:
Tags:
|
Directory:
Tags:

|


















