Tag

|
|
|

Traditional marketing for GPs is dead and a waste of money.
The information age has shifted the balance of power from GPs to patients. Today, patients use social media to share information about health providers at lightning speed, 24-7: 365 days a year and doctors can't stop it.
More telling is the fact that 35% of all patients who use social media say negative things about doctors, 40% of people who receive such negative information believe it and 41% say it affects the choices they make. Social media is the new frontier of reputation risk for doctors.
Some facts
According to a number of recent surveys, 84% of US health providers have Facebook pages, 64% have Twitter accounts, 46% post videos on YouTube, a significant percentage have profiles on LinkedIn and 12% blog. These data are indicative of what's happening in the UK. However, because doctors increasingly participate in social media doesn't mean that they are using it optimally.
Few doctors understand how social technologies interact with patients. Few use social media to reduce negative patient conversations, increase referrals, expand their services, enhance their reputations, drive loyalty and increase revenues. There are at least three reasons for this:
- Although patients increasingly engage in social media conversations, doctors don't know how to influence these
- Doctors tend to define social media technically and fail to leverage the behavioural aspects of the medium, which facilitate faster, cheaper, easier and larger scale social interactions than before
- There is no single measure of social media's financial impact, and therefore doctors find it difficult to justify allocating resources to an activity whose precise effect remains unclear.
Reputations defined by patients
Thirty three percent of all patients use social media to seek medical information, track symptoms and broadcast opinions about doctors, drugs and treatments. Age is a factor: 50% of seniors; 45% of 45 to 65 year olds and 90% of 18 to 24 year olds use social technologies to do these things. Ninety percent of everyone who uses social media trusts the health information they receive.
Although it's difficult to quantify the impact that social media has on health providers, we know that patients use social technologies throughout their entire therapeutic journeys to form opinions and help them make critical choices.
Being visible is being credible
Increasingly, patients are using social networks to obtain answers to healthcare questions and to research disease states. If a health provider has a poor internet presence, patients will question their services and expertise. A weak website with poor information will trigger huge numbers of negative conversations that tarnish reputations.
Being visible is made difficult by the size and structure of the online health market. There are over two billion websites dedicated to health in an unregulated and fragmented global marketplace. This, not only makes it difficult for health providers to gain visibility, but it frustrates and confuses patients seeking health information, which impacts on the doctor-patient relationship.
Video has become the preferred format of consumers to receive health information. Also internet browsers put a high premium on video content, so websites that use video appear higher in search hierarchies and are more appreciated by patients.
Provide what patients' want
Seventy percent of patients who search online for health information want specific answers to FAQs about disease states: symptoms, diagnosis, treatments, side effects and aftercare. Patients want access to health information at speed from anywhere, any time and anyhow. Smartphones are fast becoming the gateway to health information.
Patients prefer health information in video format because it delivers a human-touch that digitalized written words don't.
Elevate the role of patient insights
Generating rich patient insights is challenging, but important. Doctors can use social media to "listen" to patients across a few, but significant touch points of their therapeutic journeys and respond quickly to signs of changing patient needs. And this can be achieved at much less cost than what traditional communications would cost.
The power and utility of social technologies hinges on participation of both health providers and patients, which suggests flatter and more responsive organisations. Creating these is challenging. And less hierarchical and more responsive organisations should not mean diminished accountability.
Boost productivity
The behavioural aspects of social media provide doctors opportunities to organise healthcare differently. For instance, using social technologies internally to communicate with colleagues transforms messages into content, which increases the efficiency of searching and results in faster and more effective collaboration.
Doctors can employ social technologies to create data and information collaboratively, which is more accurate and valuable than that collected by more traditional methods.
Takeaway
Using social media to create, develop and manage online communities of patients, payers, specialists etc can yield significant benefits for GP practices. Over time, such communities can be used to enhance patient care, respond to patients' changing needs, amplify and broadcast new services and expertise and encourage changes in the behaviour and mindsets of patients and other stakeholders.

Here's the paradox: cancer is the most preventable of all the chronic illnesses and yet the incidence of cancer growth in Africa and other developing regions of the world is of pandemic proportions, which is exacting a significant economic and social toll.
Reason 1: There is a massive difference between global spend on cancer and on infectious diseases. Although cancer claims more lives globally than HIV/AIDS, malaria and tuberculosis combined, it receives less than three percent of public and private funding from global health. The overwhelming amount goes to infectious diseases.
Reason 2: African countries lack financial clout to attack cancer. They lack epidemiological information to guide resource planning. They lack health workers. They lack the political will and they have competing healthcare demands.
Reason 3: Bad advice. For example, recently a well resourced UK global health advisory group travelled to a poorly resourced African country, which had one of the world's highest rates of cervical cancer mortality and recommended that it should improve its road transport infrastructure to enable health workers easier access to rural areas.
Narrowing the global medical knowledge gap
Sixty years ago, cervical cancer was one of the most common causes of death for western women. However, between 1955 and 1992, the cervical cancer mortality rate in affluent western countries declined by almost 70% as medical knowledge to detect and manage the disease improved. Similar outcomes are true of other forms of cancer to the point where cancer is now preventable and manageable in most developed economies.
According to Margaret Chan, Director General, World Health Organization, the exponential growth of cancer in Africa can be significantly reduced and managed by narrowing the medical knowledge gap between the develop world and African countries.
Notwithstanding, well resourced dedicated centres of global health in affluent developed countries are failing to narrow this gap and thereby failing to reduce and control the 12 million cancer cases that occur annually. If this gap continues over the next 20 years, cancer is expected to exact a significant toll in morbidity, mortality and economic cost particularly in Africa. By 2030, the number of new cancer cases each year is projected to increase to 27 million, cancer deaths to 17 million and much of the cancer burden will fall on poorly resourced African countries.
Mobile phones rather than tarmac
Narrowing the medical knowledge gap between rich and poor countries will neither be achieved by building more roads nor continuing traditional ways of communicating medical knowledge. Such means are slow, costly and ineffective. Narrowing the medical knowledge gap will only be achieved by widespread use of the most ubiquitous healthcare innovation: the mobile telephone.
Although operationally relevant, the mobile telephone is an underdeveloped healthcare application. However, in Africa, the implementation of any healthcare strategy to reduce the burden of cancer and other debilitating health conditions should not be contemplated without leveraging mobile telephony. Why? Because Africa has one of the fastest growing telecommunication infrastructures in the world.
According to a recent joint World Bank and African Development Bank Report there are 650 million mobile users in Africa, surpassing the number in the US and Europe. "In some African countries more people have access to a mobile phone than to clean water, a bank account or electricity," the Report says.
A recent Deloitte's Report suggested that between 2000 and 2012, mobile phone penetration in Africa increased rapidly from one percent to 54%. Today it is over 60%. The main catalyst for this explosive growth is youth. "The cell phone is their landline, ATM and email in one device. Cell phones are central to their life," says Teresa Clarke, CEO, Africa.com.
According to Maurice Nkusi from Namibia Polytechnic who designed a mobile phone-based curriculum, most African youths, "have never even used a computer, but the rapidity with which they master mobile telephony reflects the era in which they live".
Mobile telephony in Africa has narrowed divides between urban and rural, rich and poor and African youth today is the first generation to have direct access to mobile phones, which are used for communicating, transferring money, shopping, listening to the radio and mingling on social media. It is a relatively small step to integrate healthcare content on mobiles that would help prevent and manage cancer.
Africa internet use increases as costs fall
Internet prices in Africa are falling and speed is increasing thanks to fibre-optic submarine cables running along the east and west coasts of Africa and connecting many countries and millions of people.
The Eastern Africa Submarine Cable System (EASSy) is a 10,000km fibre-optic cable deployed along the east and south coast of Africa to service voice, data, video and internet needs of the region. It links South Africa with Sudan via landing points in Mozambique, Madagascar, the Comoros, Tanzania, Kenya, Somalia and Djibouti. The system also interconnects with multiple international submarine cable networks for onward connectivity to Europe, the Americas, the Middle East and Asia.
At a 2013 BRIC summit in South Africa, Andrew Mthembu, chairman, i3 Africa announced that EASSy is to be complimented by a new marine cable connecting 21 African countries with Brazil, Russia and China.
Along the West African coastline is a similar submarine fibre-optic cable, which links West African countries with Europe and brings ultra-fast broadband to a region from Seixal in Portugal through Accra in Ghana to Lagos in Nigeria and branches out in Morocco, Canary Islands, Senegal and Ivory Coast.
This existing 7,000km cable has been recently complemented by a France Telecom-led system, which uses high-speed fibre optic technology to link Europe with 18 countries along the west coast of Africa and provides the capacity to allow approximately 20 million ordinary videos and up to five million high definition videos to be streamed simultaneously, without any buffering.
Today, there are 84 million Internet-enabled mobiles in Africa, all of which can access data and rich media from the internet. By 2014, 69% of mobiles will have Internet access in Africa. In response to the burgeoning demand, African markets are rapidly transitioning from mobiles with limited data access to low-cost smartphones with access to the Internet. Chinese handsets are readily available in Africa for as little as US$20.
Takeaways
Previous HealthPad commentaries have described mHealth initiatives in Africa, but few western centres for global health have fully appreciated that medical knowledge has become mobile, digital and global. Further, they have not fully appreciated the telecommunications revolution that has taken place in Africa over the past decade. Such failures help to explain why the medical knowledge gap between the developed world and African countries has not been narrowed.
This failure is also an opportunity for centres of global health to take a lead in capturing and organising medical knowledge to assist in the management of cancer and other chronic diseases and then to leverage established telecommunications infrastructures to distribute that knowledge to where it is needed the most. What a pity that narrowing the medical knowledge gap was not a Millennium Development Goal.
Directory:
Tags:

|
Prostate cancer develops in the walnut-sized gland underneath the male bladder. It is the most common cancer, other than skin cancer and is the second leading cause of cancer-related death in men.
The disease, which often develops slowly, is different to most other cancers because small areas of cancer within the prostate are common, especially in older men and may not grow or cause any problems. This presents men diagnosed with prostate cancer with some extremely difficult choices. The statistics Prostate cancer is the second most frequently diagnosed cancer in men and the fifth most common cancer overall. One in six men will be diagnosed with the disease in their lifetime and the overwhelming majority of cases occur in wealthy countries. Each year, about 37,000 men in the UK and some 210,000 men in the US are diagnosed with prostate cancer and more than 10,000 and 28,000 respectively die each year of the disease. In the US there are over two million men living with the disease and African American men have a higher incidence of prostate cancer and double the mortality rate compared with other racial and ethnic groups. In the US about US$10 billion is spent annually on treatments for the disease. Standard treatments Traditional treatments to stop the spread of prostate cancer involve surgery and radiotherapy, which has significant side effects. Following such treatments 50% of patients experience impotence, up to 20% suffer incontinence and between one and five percent who receive radiotherapy experience pain and bleeding. |
|
|

|
In 2010, tennis legend Billie Jean King had both her knee joints replaced and it changed her life. Years playing the high-impact sport left the 39-time Grand Slam winner with joint pain and stiffness in her knees. Now at 68, she is playing tennis again. Like Billy Jean, thousands of people are opting to replace their traumatised joints and patients are fast becoming younger.
An escalating incurable and costly condition As populations age peoples' joints are increasingly affected by osteoarthritis, a painful and incurable condition. Dr Anestis Iossifidis consultant orthopaedic surgeon, Croydon University Hospital, UK, says, "Osteoarthritis is the most common disease of the joints and one of the most widespread of all chronic diseases and the most common cause of severe long term pain and physical disability". At any one time, 30% of American adults are affected by joint pain, swelling, or limitation of movement. The prevalence of osteoarthritis increases markedly with age and by 65 can be observed in over half of the American population. Worldwide an estimated 630 million people have their lives blighted by osteoarthritis. In the UK the disease affects about 8.5 million people; a figure set to double to 17 million by 2030. The condition forces 33% of sufferers to retire early and each year this is estimated to cost the UK economy £3.2 billion. |
|
|
|
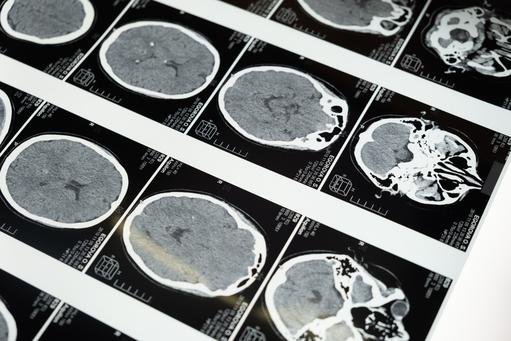
Two years ago, Ben Brabyn, a forty year old former British Royal Marine and investment banker turned entrepreneur, visited his doctor with headaches that another doctor had diagnosed as sinusitis. The second doctor suspected a brain tumour and immediately called for an ambulance to take Ben to Charing Cross Hospital, London. Scans showed a fist-sized tumor on the right side of his forehead, see above. Undetected, Ben's tumor could have killed him within days
Any brain tumor is serious and life-threatening because of its invasive nature in the limited space of the intracranial cavity. The threat a brain tumor poses depends on its type, invasiveness, location, size and the state of its development. A tumor may be particularly deadly because it can push against or invade important parts of the brain, as well as cause a lot of swelling that can result in blackouts, fits and other serious health challenges. Within hours of being admitted to hospital, surgeons removed a large panel of bone over Ben's right eye and excised his tumor, which turned out to be a benign meningioma. Most meningiomas are benign and tend to be more common in middle-aged or elderly women than in men. Ben is now fully recovered. Brain tumor deaths are increasing Each year, around 165 million people in Europe are affected by some form of brain-related disorder, which suggests that almost every family in Europe is likely to be affected. Not everyone however will be as lucky as Ben Brabyn. In the US, over 688,000 people are living with primary brain tumors, some 138,000 are malignant and about 550,000 are non-malignant. Since 2004 the incidence of brain tumors in the US has increased by 10%. In 2013 in the US, an estimated 70,000 new cases of primary brain tumors are expected to be diagnosed. In 2012 an estimated 13,700 deaths were attributed to primary brain tumours. Brain tumors are the second-leading cause of cancer deaths in American children. In 2013, approximately 4,300 Americans younger than 20 will be diagnosed with primary brain tumors. In the UK the situation is equally bleak. Over 9,000 people are diagnosed with brain and spinal cord cancer annually and it kills nearly 5,000. Over the past decade there has been a 16% increase in brain tumor deaths. The largest group of primary brain tumors is gliomas; a broad term that includes all tumours arising from the gluey supportive tissue of the brain. These make up 30% of all brain and spinal cord tumors and 80% of malignant brain tumours. |
|
|

|
|
|
|
Directory:
Tags:
What does King Fadh of Saudi Arabia have in common with the rock star Meat Loaf?
Both frequently urinated, had insatiable thirsts, were often tired and always wanted to eat. In addition they both probably were irritated by itchy feet and blurred vision. Symptoms shared by the Lord Kennedy of Southwark who, in a 2011 House of Lord’s debate, admitted that, “For many years I felt stressed, agitated, tired and run down.” King Fahd, Meat Loaf and the Lord Kennedy all suffered from diabetes, the silent epidemic.
Diabetes mellitus is a group of metabolic diseases characterized by hyperglycaemia resulting from defects in insulin secretion, insulin action or both. The disease has been recognized for more than 3,500 years, since its early description in 1552 BC in Papyrus of Ebers from Egypt. Type 1 diabetes is an absolute deficiency of insulin secretion, which results from the body’s immune system attacking insulin producing islet cells. Type 2 diabetes results from a combination of resistance to insulin action and inadequate insulin release. About 95% of the incidence of diabetes is Type 2, which is strongly associated with obesity and lack of physical activity. Another type of diabetes is called gestational diabetes, which occurs in pregnancy and shares similar features to Type 2 Diabetes.
The non-dramatic, insidious and chronic nature of the major form of diabetes masks the fact that it has become a global epidemic with the potential to overwhelm national health systems if nothing is done to halt its progress. More worrying, is the fact that Type 2 Diabetes is strongly associated with other chronic diseases such as high blood pressure, stroke, heart disease and high cholesterol. It is “a strange world” said the Lord McColl of Dulwich in the 2011 parliamentary debate: “Half the world is dying of starvation; the other half is gorging itself to death.In the United Kingdom there are over two million people suffering from diabetes as a result of obesity . . . . . diabetes has reached epidemic proportions and now affects teenagers and young children. Parents seem to be unaware and unconcerned that their children are obese.”
Lord McColl’s sentiment is echoed in a 2012 World Health Organization Report: between 1980 and 2008 obesity doubled and today 0.5 billion people, 12% of the world’s population, are obese, which is a leading cause of Type2 diabetes. Currently, over 347 million people worldwide have diabetes; an estimated 3.4 million people died from diabetes in 2004 and by 2030 diabetes is expected to increase by 150% in developing countries. Research, predicated on 30 years of data from 200 countries and regions and published in The Lancet in July 2011, confirms that the prevalence of diabetes has reached epidemic proportions worldwide despite the fact that the disease and its complications can be prevented by a healthy diet and regular physical activity. Both studies predict a huge and escalating burden of medical costs and physical disability as the diabetes increases a person’s risk of heart attack, kidney failure, blindness and some infections.
Earlier this year, a paper delivered to the American Diabetes Association at the world’s largest diabetes conference in Philadelphia, estimated the cost of diabetes, in the US alone, to be over US$174 billion and by including gestational and undiagnosed diabetes, the cost could exceed US$218 billion. Such staggering costs and the millions of sufferers represent significant drivers of research for a cure. However, the success in diabetes research has been in the treatment and a cure has been elusive. The current gold standard therapy is strict glycemic control in order to minimize complications. The therapeutic goal is normoglycemia, achieved with supplementary insulin or other pharmacological agents that either stimulate insulin release or reduce insulin resistance.
What does the future hold for a person with diabetes? Current therapies, including insulin, are not cures, but are merely palliating the consequences of defective glucose regulation. In 2011, the Lord Crisp, who has played a leading role in raising awareness about the plight of diabetes, tabled an important House of Lord’s debate, mentioned above, on chronic non-communicable diseases and argued that, “We need this debate to talk about what needs to be done to tackle the worldwide epidemic of these preventable diseases, as traditional methods of combating them are obviously no longer working.”
A potential cure for diabetes is to replace the function of defective pancreatic islets. This may be achieved directly, through islet cell or pancreas transplantation or indirectly, through a bio-artificial pancreas. Islet cell transplantation involves injecting islet cells from a donor into the liver of a patient. Usually, pancreas transplantation is achieved in the setting of a combined pancreas and kidney transplant in patients with advanced diabetes and kidney failure. In appropriate patients, both are successful options to restore normalise glucose levels in diabetic patients. However, impediments to the success of transplantation include surgical risks, costs, risks from life-long immune suppressants and eventual graft failure. Moreover, transplantation is severely limited by the relatively small number of donors compared with the demand. Over the past decade, the number of organ donors generally has increased in some developing countries. However, there are unresolved ethical and clinical issues associated with this rise in organ donors.
A promising area of diabetes research is cell engineering. This involves the generation of glucose-responsive insulin-producing cells from a diabetic patient’s own cells, which can then be implanted into the same patient without the need of donors or life-long immune suppression. However, there are significant challenges associated with this approach. From a different perspective, biotechnologists have been attempting to develop an artificial pancreas that can detect changes in glucose and deliver insulin in response to this. Although insulin pump technology has been around for many years and recently glucose sensor technology has developed significantly, there remain substantial challenges to developing a sophisticated bio-artificial pancreas that can replicate biology with the changing demands of the human body.
A successful surgical therapy for Type 2 diabetes is gastric bypass surgery. This involves changing the plumbing of the gut so that ingested food is delivered to more distal parts of the gut more rapidly after a meal. Certain forms of this surgery can have dramatic effects on improving and even completely resolving diabetes in obese diabetic patients. Although this may appear an ideal solution, surgical costs and risks cannot be ignored. Furthermore, long-term outcomes from these irreversible procedures are still unclear. Interestingly, the improvement in diabetes occurs before weight loss. This has prompted extensive research into the biological mechanisms causing improvement of diabetes following gastric bypass surgery. Gut hormones are thought to be key players in this regard. It is hoped that judicious use of a combination of gut hormones may recreate a surgical bypass using drugs without the risks, costs and irreversibility of surgery.
Although advances in diabetes research are significant, the horizon for a cure is still distant. Moreover escalating costs of delivering medical cures to increasing numbers of patients and risks associated with some of the potential options are significant hurdles. At this moment in time, the best option for a cure for diabetes seems to be prevention.
Over the last century, our genes and biology have not changed much, but our lifestyles certainly have. Changes in the way we live our lives appear to have occurred in tandem with a diabetes and obesity explosion. It is difficult to ignore the fact that this chronic non-communicable epidemic has societal and environmental origins that need to be addressed more effectively while we wait for a biomedical cure. Former FDA Commissioner David Kessler suggests that diabetes may not be an entirely self-inflicted phenomenon. In his book, The End of Overeating, Kessler warns that restaurants and food processors purposely engineer food that encourages people to overeat and ruin their lives. But, if you do not warm to conspiracy theories, think of the Chinese proverb: "He that takes medicine and neglects diet, wastes the skills of the physician.

|
|
|

|
|
|





