
|
|
|
|
|

| Since we first published this Commentary just over a year ago it’s received over 10,000 views. We’re republishing it as colleagues have suggested that the digitization of MedTech is more relevant today because of the impact CoVID-19 has had on the industry. |
|

|
|
|
|
|
- The CoVID-19 pandemic created an unprecedented global shock and killed hundreds of thousands
- Nations responded by closing their borders, implementing stringent lockdowns and saying the world is at war with a common invisible adversary
- Responses to the outbreak diverged in the different regions of the world
- Asian countries responded rapidly and effectively
- The US and UK responded slowly and ineffectively
- Observers suggested that the divergent responses to CoVID-19 signal a shift in power and influence from West to East
- National responses alone are insufficient to effectively deal with the coronavirus
- Only by embracing effective international cooperation will governments protect their citizens and safely exit the CoVID-19 crisis
National leaders have described the coronavirus CoVID-19 pandemic as “the enemy”. In attempts to protect their citizens, nations turned inwards and closed their borders, implemented stringent lockdown restrictions and suggested that the world is at war with a common adversary it cannot see. The speed and effectiveness of national responses to the new coronavirus crisis differed, but not even the wealthiest, most advanced nations were able to protect their citizens. The global coronavirus crisis made millions seriously ill, killed hundreds of thousands, destroyed industries, bankrupted thousands of companies, caused economies to nose-dive and threw societies into turmoil. Only by avoiding nationalist policies and embracing effective international cooperation will governments protect their citizens and safely exit the CoVID-19 crisis.
Viruses are notoriously difficult to treat and cure
CoVID-19 has rapidly spread throughout the world with a scale and a severity not witnessed since the devastating Spanish Flu in 1918. So-called because Spain was neutral during WW1 and was one of the few countries where journalists were free to report on the outbreak. In an era before antibiotics and vaccines, the Spanish Flu claimed the lives of nearly 0.68m Americans, 0.25m Britons and between 50 to 100m people worldwide. Adjusting for population growth, that is equivalent to between 200 and 425m today.
At the time of writing - June 2020 - neither an adequate therapy nor a vaccine has been developed and CoVID-19 remains prevalent in populations throughout the world. Even with today’s scientific advances, infectious diseases are notoriously challenging to either treat or cure: an Ebola vaccine was more than two decades in the making; despite the first cases of the human immunodeficiency virus (HIV) presenting in 1983, we still do not have a therapeutic preventative vaccine for the disease; nor do we have a vaccine for severe acute respiratory syndrome (SARS), a killer coronavirus, which also originated in China and was unknown before its outbreak in 2002.
Recovery will neither be straightforward nor quick
Notwithstanding, governments have lifted lockdown restrictions in order to get their economies working again. V, U, W and L are letters of the alphabet used to describe the shape of a recovery following the economic crisis caused by CoVID-19. Stringent lockdowns forced economies into unprecedented cold storage, and no one knows what shape a recovery will take since professional forecasters have never encountered anything like the sheer magnitude of the current economic crisis.
The Bank of England’s Monetary Policy Report published in May 2020, warned that the coronavirus has caused the worst economic crisis in 300 years. So, emerging from this is unlikely to be either straightforward or quick. National responses to the coronavirus outbreak were mixed. Although it is too soon to know the longer-term effects of the virus, China, Singapore and South Korea are among the countries that responded early and effectively, while the US and UK, together with other Western European countries, responded late and less effectively. As of June 1, China, with a population of 1.4bn, had 83,017 confirmed cases and 4,634 deaths; South Korea with a population of 52m, had 11,537 cases and 270 deaths, and Singapore with a population of 5.7m, had 34,884 confirmed cases and 23 deaths.
In this Commentary
This Commentary describes the divergent national responses to the CoVID-19 pandemic; in particular that of China, Singapore, South Korea, the US and UK. China’s more effective response might have been because Beijing benefitted from the lessons it learned after the SARS epidemic in 2002. Governments also differed in their approaches to lifting restrictions. China’s approach was slower than that of the US and more determined to make some of the unexpected benefits thrown up by the crisis permanent. Some observers perceive such variances as a difference between liberal and illiberal nations. Others view the divergences as a shift in power and influence from West to East. We suggest that the divergent responses and outcomes are a product of the capacity and legal authority of different states and reveal different mindsets and competing views about solutions. We also contend that the devastation created by the pandemic will only be resolved with effective international cooperation. However, it is difficult to see this happening in the near term as the pandemic has become a theatre for a wider political disagreement between the US and China, in which other nation states are being forced to take sides.
Asian nations won the battle against CoVID-19
China, Singapore and South Korea leveraged the collectivists mindset of their citizens, their centralised authority and digital infrastructures to quickly implement the gold standard “test-trace-and-isolate” strategy to reduce and control the virus. The reason for such prompt actions and the subsequent relatively low number of cases and deaths in these Asian countries is described by Byung-Chul Han, a South Korean-born German Professor of Philosophy at the Universität der Künste in Berlin. In an article published on May 22, in the Spanish newspaper El Pais, Han suggests that Asian nations won the battle against the CoVID-19 outbreak because their citizens, “have a collectivists mindset, which comes from their cultural tradition of Confucianism. Asians are less rebellious and more obedient than people in the West. They trust the state more. Daily life is much more organised, and Asians are strongly committed to digital surveillance. The epidemics in Asia are fought not only by virologists and epidemiologists but also by computer scientists and big data specialists”.
Confucian mindset rather than authoritarianism
Given Iran’s response to CoVID-19 has been less effective, it seems reasonable to suggest that the Confucian mindset, rather than authoritarianism, appears to provide at least a short-term advantage. In early March, at the Shia Muslim Masumeh shrine in the holy city of Qom, pilgrims licked and kissed its gates. Qom experienced Iran’s first outbreak of the coronavirus and became the country's worst-hit city. Shortly afterwards the government closed all major Shia shrines across the Islamic republic and reopened them again in late May. As of June 1, Iran with a population of 81m, had confirmed 154,000 cases of CoVID-19 and 7,878 deaths.
|
|
|
|

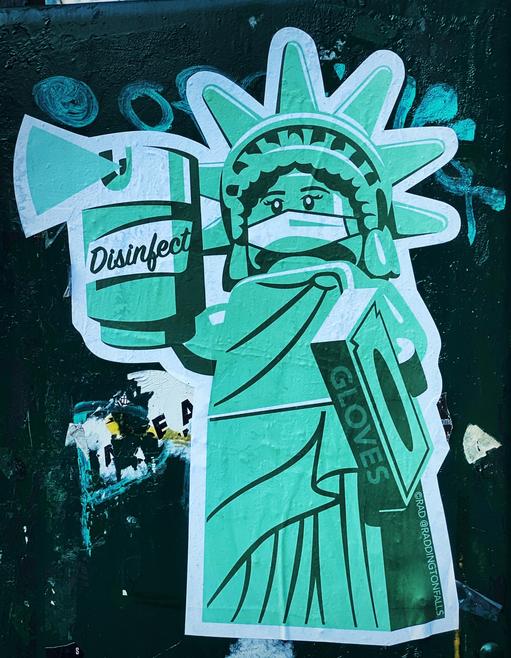
The HealthPad team extends Ramadan Mubarak to all our friends, family members and colleagues who are participating in the Holy Month of Ramadan. We very much would like to share with you a short video by DrSufyan Hussain, Consultant Physician in Diabetes and Endocrinology at Guy's and St Thomas' NHS Foundation Trust, London, UK, which we made to specifically help those who are living with diabetes and fasting.
During these unprecedented challenging times caused by the coronavirus CoVID-19 pandemic, we trust that you all stay safe and well and let the spirit of Ramadan remain in your hearts and light up your souls from within.
During these unprecedented challenging times caused by the coronavirus CoVID-19 pandemic, we trust that you all stay safe and well and let the spirit of Ramadan remain in your hearts and light up your souls from within.

The HealthPad team extends its sincerest best wishes to you, your families and loved ones during these unprecedented times caused by the coronavirus CoVID-19 pandemic. We trust that you all stay safe and well.
To everyone working long and stressful hours on the frontline of healthcare; thank you for the sacrifices you’re making every day to help others in their moments of need. Your dedication, commitment and courage have our deepest gratitude and admiration.
Also, our heartfelt thanks go to all key workers who are unselfishly providing essential services, which are helping all of us through this coronavirus outbreak. Your resolution and mettle make a huge difference to our daily lives and we hold you in the highest esteem.
To everyone working long and stressful hours on the frontline of healthcare; thank you for the sacrifices you’re making every day to help others in their moments of need. Your dedication, commitment and courage have our deepest gratitude and admiration.
Also, our heartfelt thanks go to all key workers who are unselfishly providing essential services, which are helping all of us through this coronavirus outbreak. Your resolution and mettle make a huge difference to our daily lives and we hold you in the highest esteem.
#coronavirus #CoVID-19 #frontlinehealthcareworkers #keyworkers #healthcare
Directory:
Tags:

- The coronavirus CoVID-19 has created the greatest health-cum-economic-cum-societal crisis in history and put unprecedented pressure on overstretched and unprepared healthcare systems
- Before the coronavirus outbreak, primary care in England already was in crisis, fuelled by an aging population, a large and increasing demand for its services and a shrinking supply of health professionals
- In 2019, before the outbreak, 75% of primary care doctors (GPs) across 540 clinics in England were over the age of 55 and nearing retirement and a large percentage of newly trained GPs were seeking employment abroad
- Patients who could not get GP appointments used A&E departments as convenient drop-in clinics for minor ailments, which significantly increased healthcare costs and burden
- For decades successive UK governments have tried in vain to transform the nation’s primary care services predicated upon face-to-face patient-doctor consultations
- Several well-funded long-term national plans advocated increased digitization of some routine primary care services
- But before the coronavirus outbreak only 1% of all primary care consultations were online
- What these national plans could not achieve in decades appears to have been achieved in days by the UK’s NHS’s response to the coronavirus outbreak
- Today, millions of patients in England are having face-to-face appointments with their GPs replaced by telephone or video consultations
- Could CoVID-19 transform the UK’s traditional primary care model?
Introduction
The UK’s National Health Service’s (NHS) response to the coronavirus CoVID-19 outbreak might improve the nation’s crisis ridden primary care service. This became evident in March 2020, when the UK government ordered all citizens except key workers to stay at home. At the same time, NHS England announced its ‘battle plan’ for CoVID-19, which recommended that England’s 7,000 primary care clinics start conducting as many remote consultations as soon as possible. In a matter of days, millions of patients had face-to-face appointments with their GP replaced by telephone or video consultations. If this shift to online consultations becomes permanent then the NHS’s response to the coronavirus would have achieved in days what well-funded national healthcare plans, such as the NHS Digital First Primary Care drive, could not achieve in decades.
Future healthcare is digital
For years, the benefits of online doctor-patient consultations have been advocated by Devi Shetty, a world-renowned heart surgeon and founder and chairman of Narayana Health, one India’s largest hospital groups. According to Shetty, “The next biggest thing in healthcare is not going to be a ‘magic’ pill, a faster scanner or a new operation but information technology (IT). IT will dramatically change the way a health professional will interact with a patient. Every step of patient care will be informed by a protocol embedded in a smartphone. This will make healthcare safer for the patient and remove a lot of traditional dace-to-face healthcare activities and shift healthcare away from the clinic and into the home. Doctors and patients don't need to be together; they could be in their respective homes and effective consultations could take place online.” (see video below)
The next ‘big thing’ in healthcare
The coronavirus CoVID-19
In this Commentary
UK’s primary care crisis
Changing and aging population
Shrinking supply of GPs
Failing national initiatives to improve primary care
The UK’s NHS
National plans to improve the NHS
NHS long term plans and private online healthcare solution companies have delivered little change
The plan emphasises the importance of developing digital services, and recommends that within five years, all patients should be able to access GP consultations via a telephone or online. This goal is supported by NHS Digital, which is the national information and technology partner to the UK’s health and social care system. Its mission is to harness the power of information and technology to improve healthcare. Over the past decade there has been an increasing number of innovative online private healthcare solutions companies entering the market. (see below). Notwithstanding, these and the NHS’s well-funded national plans, have failed to dent the primary care crisis by slowing the vast and escalating demand for healthcare and reversing the shrinking supply of healthcare professionals. So, for the past two decades at least, the NHS has tended to operate on the cusp of a crisis.
The death of distance

A doctor only needs to touch a patient if s/he is going to operate on that patient
Innovative online healthcare solution enterprises
Technologically heavy and strategically light
A Chinese example
Takeaways
The coronavirus CoVID-19
In December 2019, initial reports of a new coronavirus - CoVID-19 - emerged when patients from Wuhan, the sprawling capital city of China’s Hubei province, which has a population of some 11m, presented with pneumonia of unknown origin. By December 2019 the virus had spread to other countries and on 11th March 2020, the World Health Organization characterised the outbreak as a pandemic. CoVID-19 is an illness caused by a member of the coronavirus family that has never been encountered before but is believed to come from animals.There have been other coronaviruses. For example, severe acute respiratory syndrome (Sars) and Middle Eastern respiratory syndrome (Mers) are both caused by coronaviruses that came from animals. In 2002, Sars spread virtually unchecked to 37 countries, causing global panic, infecting more than 8,000 people and killing about 800, but it soon ran itself out. Mers first emerged in 2012, cases of which have been occurring sporadically since. Mers appears to be less easily passed from human to human, but has greater lethality, killing 35% of about 2,500 people who were infected. CoVID-19 is different to Sars and Mers in that the spectrum of disease is broader, with around 80% of cases leading to a mild infection. There may also be many people carrying the disease and displaying no symptoms, making it even harder to control. CoVID-19 affects your lungs and airways and can cause pneumonia. So, people with an inflammatory lung disease that causes obstructed airflow from the lungs, such as asthma and chronic obstructive pulmonary disease (COPD), are particularly vulnerable; as are people with weak immune systems, which make them susceptible to infections that might be more severe or harder to treat. In January 2020, China’s national health commission confirmed human-to-human transmission of CoVID-19, and there have been such transmissions in countries throughout the world. Those who have fallen ill are reported to suffer a general feeling of being unwell, fever, dry cough, tiredness, breathing difficulties and a loss of taste and smell. In roughly 14% of cases the virus causes severe disease, including pneumonia and shortness of breath. In about 5% of patients it is critical, leading to respiratory failure, septic shock and multiple organ failure. As this is viral pneumonia, antibiotics are of no use. The antiviral drugs we have against flu will not work. Recovery depends on the strength of your immune system. Many of those who have died were already in poor health. Initially, scientists were challenged to accurately assess how dangerous CoVID-19 was because there were inadequate data. A challenge to collecting data was because of a shortage of tests and also because people who had contracted the coronavirus were emitting, or “shedding,” infectious viruses early in the progression of the illness; sometimes before they develop symptoms.
The 1918 Spanish Influenza remains the most devastating virus in modern history. The disease swept around the globe and is estimated to have caused between 50m and 100m deaths. A cousin of the same virus was also behind the 2009 swine flu outbreak, thought to have killed as many as 0.58m. Other major viral outbreaks include the Asian flu in 1957, which led to roughly 2m deaths and the Hong Kong flu, which killed 1m people 11 years later.
The 1918 Spanish Influenza remains the most devastating virus in modern history. The disease swept around the globe and is estimated to have caused between 50m and 100m deaths. A cousin of the same virus was also behind the 2009 swine flu outbreak, thought to have killed as many as 0.58m. Other major viral outbreaks include the Asian flu in 1957, which led to roughly 2m deaths and the Hong Kong flu, which killed 1m people 11 years later.
In this Commentary
This Commentary is produced by HealthPad, which is an online health solutions company. (see below). We begin the Commentary by briefly describing the underlying reasons for the UK’s primary care crisis, which include: (i) the changing and aging population and the consequent increased demand for healthcare, (ii) the shrinking supply of health professionals, and (iii) failing national initiatives to improve the provision of primary care. We then draw attention to some well funded national plans, whose intentions have been to harness the power of information and digital strategies to reform and improve primary care services in England. We also cite research, which suggests that these plans have failed. The Commentary briefly describes a number of innovative online healthcare solution companies, (HealthPad is one). The majority of these are private initiatives, which have taken advantage of the UK’s high smartphone penetration rates and advanced wireless networks to enter the UK’s healthcare market with an intention to transform the sector. Notwithstanding, to-date the overall impact of these companies has been marginal, due in part, to the general resistance of private enterprises playing a significant role in England’s public NHS, which offers free healthcare to all citizens at the point of care. However, they represent a nascent UK online healthcare solutions market, which is well positioned to benefit from the nation’s response to the coronavirus outbreak, which has forced more primary care services to be delivered online. To increase their footprint these companies, which are largely driven by technology, will need to become more strategic and consolidate. And this will take time. We conclude the Commentary by looking to China and WeDoctor to understand the potential that online services can make to the delivery of healthcare in England. WeDoctor is a Chinese mobile app launched in 2010 to help patients book doctor appointments. Over the past decade it has added more functions to help unclog China’s fragmented and bureaucratic healthcare system and has become a US$5.5bn healthcare company, which connects some 210m registered users with 360,000 doctors.
UK’s primary care crisis
There are three drivers to the UK’s primary care crisis: (i) the changing and aging population, which increases the demand for healthcare, (ii) the shrinking supply of healthcare professionals to a point where GP workloads are becoming unsafe, and (iii) failing national initiatives to improve the provision of primary care. Let us briefly describe these.
Changing and aging population
The UK’s population is changing and aging, which is fuelled by improvements in life expectancy and a decrease in fertility. According to the UK’s Office of National Statistics, in 2016, there were 12m UK residents aged 65 years and over, representing 18% of the total population. 25 years before, in 1991, there were 9m, accounting for 16% of the population. By 2040, it is projected that there will be an additional 8m people aged 65 years and over in the UK: a population roughly the size of present-day London, which will account for 25% of the total population.
A report by Deloitte, a consultancy, suggests that as people age so their propensity for illness increases and more than a quarter of the UK’s population of some 66m have long-term chronic illnesses. This places a significant extra burden on the nation’s overstretched primary care services by utilizing about half of all GP appointments. Deloitte’s analysis is supported by a British Medical Association’s 2019 GP Patient Survey, which found that GP clinics are now caring for 0.72m more patients than they were in 2018. Findings of a 2016 report by the UK’s Royal College of General Practitioners (RGCP), suggest that GPs see 1.3m patients a day and do more than 370m consultations annually: 60m more than in 2010. A research study on GP productivity carried out by the King’s Fund and also published in 2016, suggested that between 2010 and 2015 the total number of telephone consultations increased by 15%, but still only accounted for 1% of all patient-doctor consultations.
Shrinking supply of GPs
As the UK’s population has grown and aged and the consequent demand for healthcare has increased, so there has been a sustained fall in the number of GPs. This dynamic is described in a Nuffield Trust report published in May 2019, which confirms the findings of a joint report from the Institute of Fiscal Studies and the Health Foundation for the NHS Confederation, which concluded that, “The fall in GPs per person reflects insufficient numbers previously being trained and going on to join NHS England, failure to recruit enough from abroad and more GPs leaving for early retirement”. As to the future, a 2019 report by three leading think tanks - the Nuffield Trust, the Health Foundation and the King's Fund - predicts that GP shortages in England will almost triple to 7,000 by 2024. According to NHS Statistics, Facts and Figures, currently there are just over 42,000 GPs working in England, down by nearly 1,500 since 2016.
Failure to stop or slow these trends means today, primary care services in England struggle with staff shortages and a rising demand for care. A 2019 Pulse Magazine survey found that GPs in England are seeing more patients than is safe. A probe undertaken by The Times in 2019 suggested that the national shortage of GPs has left some surgeries with one permanent doctor caring for as many as 11,000 patients and one in 10 GPs are seeing up to 60 patients a day, double the number considered safe.
GPs across the UK work an average 11-hour day. In that time, they typically see patients for 8 hours and spend the other 3 on administrative tasks such as checking test results and reading letters sent by hospitals. A 2019 British Medical Association survey found that more than 80% of GPs said the pressure to attend to multiple tasks at once meant they were unable to guarantee safe care, while 91% said excessive workload was the main reason the NHS was struggling to recruit enough staff. The situation has resulted in patients having to wait longer - up to three weeks - for a GP consultation. It seems reasonable to suggest that GPs with too many patients and using traditional face-to-face delivery methods will fail in their duty of care, which obliges them to inform patients about their health and reach shared clinical decisions about treatments. This requires that patients understand their condition/s and are well informed. In many cases, a 10-minute face-to-face GP consultation might not be the best way to achieve this.
Failing national initiatives to improve primary care
Subsequent UK governments have struggled to reduce the primary care crisis with well funded national plans. In 2019, the British Medical Journal published findings of a survey to report UK GPs’ views and experience of national healthcare initiatives introduced in England to address the workforce crisis in general practice. The survey was conducted in the same region as a similar survey undertaken in 2014. This allows for a comparative analysis to see how GPs’ views have changed over time. Findings confirm that primary care in England remains in crisis and suggest that numerous national initiatives to improve general practice are perceived by GPs as, “reactive in approach”. To reduce the primary care crisis, respondents suggested, “more GPs and better education of the public".
The UK’s NHS
Healthcare in the UK is mainly provided by the National Health Service (NHS), which is a vast public institution funded largely from general taxation to the tune of some £134bn (US$161bn) a year. Created in 1948, the NHS provides free health services at the point of care for everyone living in the UK and has become the largest single payer health system in the world, and the biggest employer in the UK with 1.2m full time equivalent (FTE) workers, which is the fifth-largest workforce in the world. NHS England is a vast bureaucratic and fragmented organisation, which has proven difficult to change. Private provision of NHS services has always been controversial, even though some services, such as dentistry, optical care and pharmacy, have been provided by the private sector to the NHS for decades and most GP practices are private partnerships. It is challenging to determine how much the NHS spends each year on the private sector because central bodies do not hold detailed information on individual contracts with service providers, especially where these contracts may cover relatively small amounts of activity and spending. Notwithstanding, estimates suggest the share of the NHS’s total revenue budget that is spent on private providers is about 7.3%.
National plans to improve the NHS
The planning and authorising of NHS services is the responsibility of regional Clinical Commissioning Groups (CCGs). Although CCGs are constantly changing because of mergers, as of 2019, there were 191 CCGs in England supporting about 7,000 primary care clinics, some 42,000 GPs and about 15,800 FTE nurses who work in GP clinics, and 1,257 hospitals, which include NHS Trust-managed hospitals and private hospitals that provide services to the NHS. In total, the NHS employs around 150,000 doctors and over 320,000 nurses and midwives.
Successive UK governments have been aware of the impact of technological advances, changing healthcare needs and societal developments on healthcare and have introduced a succession of well-funded national plans to change and improve the NHS. For example, in June 2018, the UK’s Prime Minister announced a new five-year funding settlement for the NHS that amounted to an extra £20.5bn (US$25.2bn) between 2019 and 2024, which represents a 3.4% real average annual increase.
NHS long term plan to transform primary careTo unlock the funding, national bodies were asked to develop a long-term plan to help the NHS cut costs and improve services. The suggested plan articulated the need to integrate care in order to meet the needs of a changing population and was in line with the Forward View, a planning document published in 2014 and the General practice forward view,which was first published in 2016 and updated in subsequent years. The long-term plan committed the government to an extra £2.4bn (US$3bn) a year to speed up the transformation of primary care and suggested GP clinics join together to form networks typically covering 30,000 to 50,000 patients and provide them with multidisciplinary integrated care. The plan also suggested ‘significant changes’ in the existing performance management and payment of NHS GPs [the Quality and Outcomes Framework (QOF)] in order to encourage more personalised care.
NHS long term plans and private online healthcare solution companies have delivered little change
Three of five principal objectives of the latest NHS long term plan are to: (i) “give people more control over their own health and the care they receive”; (ii) “increase the contribution to tackling some of the most significant causes of ill health, including new action to help people stop smoking, overcome drinking problems and avoid Type 2 diabetes”, and (iii) “provide more convenient access to services and health information for patients”.
The plan emphasises the importance of developing digital services, and recommends that within five years, all patients should be able to access GP consultations via a telephone or online. This goal is supported by NHS Digital, which is the national information and technology partner to the UK’s health and social care system. Its mission is to harness the power of information and technology to improve healthcare. Over the past decade there has been an increasing number of innovative online private healthcare solutions companies entering the market. (see below). Notwithstanding, these and the NHS’s well-funded national plans, have failed to dent the primary care crisis by slowing the vast and escalating demand for healthcare and reversing the shrinking supply of healthcare professionals. So, for the past two decades at least, the NHS has tended to operate on the cusp of a crisis.
According to Deloitte, the UK has more than 90% smartphone penetration. The main driver of high smartphone adoption rates is the take-up among older age groups. By 2023 smartphone ownership among 55-to-75-year-olds will reach 85% in the UK, and the difference in smartphone penetration by age will disappear. Further, the UK’s smartphone market has seen a greater variety of choice of models and the introduction of faster and more reliable wireless networks. This has benefited the online private healthcare solution companies, which have entered the UK market to provide varying degrees of qualified online healthcare information, consultations, networking opportunities, triage and Q&A. According to Shetty, “A doctor only needs to touch a patient if s/he is going to operate on that patient. If a doctor doesn’t need to operate, a doctor-patient consultation can take place remotely. For a patient-doctor communication distance doesn’t matter.” (see video below)

A doctor only needs to touch a patient if s/he is going to operate on that patient
Innovative online healthcare solution enterprises
The new online healthcare solution enterprises are a combination of private, public and charitable initiatives, which are well positioned to contribute to the transformation of the UK’s traditional primary care model and include: Babylon Health, which provides remote consultations with doctors and healthcare professionals via text and video; BioBeats, a workplace wellbeing platform designed to empower and improve mental health; Docly, a digital messaging healthcare service, which is a spin-off of Min Doktor; Doctorlink, which partners with payers, healthcare professionals and pharmacists to provide a 24-7 platform for NHS patients to assess symptoms; DrDoctor, a patient engagement platform, which enables patients to book, change and cancel their appointments; EggPlant, a software testing and monitoring company, which helps to streamline patient activities; Dr Fox, an online primary care clinic and pharmacy service; Gogodoc, an online GP video consultation service with possible follow-up home visits; Healthcare Communications UK, which provides appointment management software and patient experience surveys; HealthPad, an online platform that manages and distributes healthcare video information between health providers and patients in order to improve outcomes and cut costs, and has accrued a proprietary content library of over 6,000 short videos contributed by leading clinicians that address peoples FAQs across some 30 therapeutic pathways, (HealthPad is the publisher of this Commentary). HealthTalksOnline, an events and community portal for health; HealthUnlocked, a social networking service that offers peer support to help people manage their health; Healum provides healthcare professionals with a software, which enables them to support and motivate their patients to better manage their conditions; LIVI, provides GP video consultations; Medshr, a platform for medical professionals to discover, discuss and share clinical cases and medical images; Microtest Health, a health informatics company that provides practice management systems for NHS GP surgeries. MSKnote Limited creates clinical applications for healthcare professionals and patients with a focus on musculoskeletal conditions; MyWay Digital Health provides advice and solutions to help patients better manage diabetes; NHS.uk/conditions provides online text-based information and advice about medical conditions; NHS 111, a free-to-call medical helpline; the Now Healthcare Group, a GP video consultation platform and tele-pharmacy; Patient Access, which started by enabling patients to book GP appointments online and order repeat prescriptions and has evolved to allow patients to connect with their GPs remotely and access their medical records online; Patientinfo provides patients and health professionals with online health information. PatientAccess and Patientinfo are subsidiaries of EMIS Health, a leading supplier of software used by NHS England; Patients Know Best, a social enterprise, which provides patients with access to their medical records and information about treatments; PatientsLikeMe, an online service that helps patients find people with similar health conditions in order to take actions that are expected to improve outcomes; Push Doctor, an online video consultation service; SaySo Medical is a digital communications agency, which connects people in order to improve their health; SystmOne, a centrally hosted computer system that provides primary care professionals with electronic patient health records in real time at the point of care; uMotif, a platform that captures electronic patient-reported outcomes data across a range of conditions and works with pharmaceutical companies to measure patient’s health, outcomes and experience; Unmind, a workplace mental health platform designed to empower organisations and employees to improve their mental wellbeing; Visiba Care, a digital solutions company, which provides communication and administration software for healthcare practices; VisionHealth provides NHS primary care professionals with software solutions; VisualDX provides clinical decision support systems to enhance diagnoses and therapeutic decisions in order to improve patient safety; WebMD, an online publisher of healthcare news and information, and Zava, an online GP and pharmacy service.
Technologically heavy and strategically light
Despite a significant number of online healthcare solution enterprises entering the market and the fact that some provide services to millions of people in the UK, this market segment is in its infancy and fragmented. All the initiatives mentioned above have been advantaged by the NHS’s response to the coronavirus outbreak. Notwithstanding, to permanently increase their footprint and significantly influence primary care in England, barriers to private enterprises and to online services will need to be reduced; and private companies in this segment will need to act more strategically and consolidate.
Most of these online healthcare service providers are technologically heavy and strategically light. For private companies in this market to grow and increase their influence on the NHS they will need to increase their focus on profitability and scale, which will require them to become more strategic and develop merger-integration skills. To become a dominant player, a company will have to successfully consolidate. Speed and merger competence are paramount. Companies that capture critical ground early and move up the consolidation curve the fastest will be successful. Enterprises that are slow to consolidate will become acquisition targets and disappear. Companies that stay out of the consolidation contest altogether will not survive.
A Chinese example
History has shown that many short-term emergency measures have a tendency to become permanent fixtures. Thus, the UK’s response to the coronavirus CoVID-19 outbreak might permanently reduce the barriers to moving routine primary care tasks to innovative private online enterprises.
In an attempt to fully appreciate the potential of increasing online primary healthcare services in England, consider WeDoctor, a Chinese mobile app launched in 2010 by artificial intelligence expert Jerry Liao. Originally called Guahao (Mandarin for “booking”), WeDoctor started as a simple booking platform that made it easier for patients to make appointments with doctors. From these humble beginnings WeDoctor grew by adding extra functions such as reminders for regular medical checks, screening, prescriptions and online diagnoses and consultations. This helped to unclog China’s fragmented and bureaucratic healthcare system and made quality healthcare more accessible to the average person.
WeDoctor secured backing from Tencent Holdings, a Chinese multinational conglomerate, Sequoia Capital, the Goldman Sachs Group and the insurer AIA Group. In 2018, the company raised US$0.5bn in a private financing round at a valuation of US$5.5bn. Today, WeDoctor has more than 210m registered users mainly in China for its online appointment booking, prescription and diagnosis services and is linked to about 3,200 hospitals and 360,000 doctors. In March 2020, at the height of the CoVID-19 pandemic, it was reported that, in the latter half of 2020, WeDoctor intends to raise HK$1bn in an IPO on the Hong Kong Stock Exchange at a valuation of HK$10bn.
Although NHS England is much smaller than China’s healthcare provision, it is similarly fragmented and bureaucratic. The UK online solutions enterprises described in this Commentary have significant potential simply by helping to reduce GPs large and increasing burden of administration while increasing the connectivity between patients and GPs. This will help GPs to concentrate on what they have been trained to do and improve healthcare for people in most need.
Takeaways
Over the past two decades, legacy primary care systems and attitudes in the UK have slowed the uptake of online healthcare solutions. Notwithstanding, the NHS’s response to the coronavirus CoVID-19 outbreak might prove to have helped to transform the UK’s traditional face-to-face primary care model by making GPs deliver some of their services online. In a recent interview with the New York Times, Dr Bruce Aylward, Assistant Director-General of the World Health Organization, stressed how the Chinese had responded to the coronavirus outbreak by significantly increasing the amount of medical care the nation provides online. In light of the discussion in this Commentary, be minded that in Mandarin the word “crisis” is denoted by two characters: 危机, one means ‘disaster’ and the other means ‘opportunity’.
#coronavirus #coVID-19 #NHSEngland #NHS #pandemic #primarycarecrisis #ChinaWeDoctor #WeDoctor #DigitalHealthcare
Directory:
Tags:

- The burden of breast cancer throughout the world is significant and increasing
- Research has shown that a cheap pill (anastrozole) halves postmenopausal women’s risk of breast cancer and continues to be effective seven years after women stop taking the drug
- Anastrozole has fewer side-effects and is more effective than comparable treatments
- Government watchdogs both in the UK and US recommend anastrozole
- But the uptake of the drug in the UK is relatively low
- Doctors are not prescribing anastrozole and women are not availing themselves of the drug
- The UK’s NHS should employ new behavioural techniques to influence and change doctors’ and patients’ decisions and increase the uptake of anastrozole to reduce the burden of breast cancer
Will behavioural techniques improve breast cancer outcomes?
Being a woman and growing older are two unavoidable risk factors for breast cancer. Indeed, most breast cancers are found in women who are 50 years or older. Despite significant advances in diagnoses and treatments, breast cancer is one of the rapidly increasing cancers among women and a significant cause of cancer-related morbidity and mortality worldwide. Breast cancer alone accounts for 30% of all new cancer diagnoses among females and has become a major 21st century health challenge.
Study shows long term benefits of a cheap breast cancer pill
Research findings reported in the December 2019 edition of The Lancet and also presented at the December 2019 San Antonio Breast Cancer Symposium in Texas, show that a cheap pill, anastrozole, if taken once a day for 5 years, not only halves postmenopausal women’s risk of breast cancer, but continues to be effective seven years after stopping treatment, which for the first time, suggests a long-term benefit.
Relatively low uptake
The UK’s NHS watchdog, the National Institute for Health and Care Excellence (NICE), suggests that hundreds of thousands of healthy older women should take anastrozole to cut their risk of breast cancer and recommends that the drug is offered to postmenopausal women at moderate to high risk of breast cancer unless they have severe osteoporosis. However, evidence suggests that some doctors in the UK are not prescribing anastrozole and some women are not availing themselves of the drug despite its demonstrated clinical benefits and the fact that anastrozole is supported by NICE.
Jack Cuzick, the lead author of The Lancet 2019 paper, who is Professor of Epidemiology and the Director of the Wolfson Institute of Preventive Medicine at Queen Mary University, London, is concerned because although anastrozole is, “An agent that looks really effective with minimal side-effects and is available on the NHS in the UK; its uptake has been quite low with only a tenth of eligible women receiving it”. Cuzick’s concerns are echoed by Delyth Jane Morgan, Chief Executive of the charity Breast Cancer Now, who said: "It is worrying to hear that anastrozole may not be being offered to all that could benefit. We need to understand the extent of this potential issue. It's essential that we raise awareness of this option among doctors and patients".
In this Commentary
Part 1 of this Commentary explores some of the reasons for the relatively low uptake of anastrozole. Part 2 describes new behavioural techniques, which could be cheaply and easily employed by health systems to increase the uptake of anastrozole and dent the burden of breast cancer. Also the Commentary: (i) describes breast cancer, (ii) provides some epidemiological facts of the disease, (iii) estimates the cost to treat breast cancer in the UK, (iv) describes hormone receptor positive breast cancer, (v) explains how anastrozole works and (vi) reports the findings of The Lancet 2019 study.
Part 1
Breast cancer
Cancer is a group of diseases that cause cells in your body to change and spread out of control. Most types of cancer cells eventually form a lump or mass called a tumour and are named after the part of your body where the tumour originates.
|
|
|
|

- Bioengineers throughout the world are competing to achieve the Holy Grail: an affordable, point-of-care blood test - liquid biopsy - that detects cancer before any symptoms present
- Success in achieving this will save millions of lives, substantially reduce healthcare costs and make investors, researchers and organisations billions
- Despite significant advances no one has yet achieved the Holy Grail and there remains a substantial gap between researchers’ aspirations and reality
- How close are we?
Finding the Holy Grail: early detection tests for cancer
“It’s too soon to even claim that the research is promising," commented Paul Pharoah, a professor at Cambridge University’s Centre for Cancer Genetic Epidemiology, on the research findings of Daniyah Alfattani, a PhD student in the Centre of Excellence for Autoimmunity in Cancer (CEAC) at Nottingham University’s School of Medicine in the UK.
Alfattani was presenting research findings of a small study at the National Cancer Research Institute’s (NCRI) conference in Glasgow, Scotland, in November 2019, which is an international forum for showcasing cancer advances.
A September 2019 HealthPad Commentary described another early detection test for breast cancer called CanRisk, which has been developed by researchers from Cambridge University’s Centre for Cancer Genetic Epidemiology and has the potential to identify women with different levels of risk of breast cancer.
Alfattani and bioengineers from the universities of Nottingham and Cambridge are players in a vast and rapidly evolving international army of researchers engaged in an intensely competitive global race to develop an affordable, point-of-care, early detection test (EDT) for cancer based upon a liquid biopsy and next generation sequencing technologies. The Holy Grail is for such a test to detect cancer cells in an asymptomatic patient, locate the tissue of origin and give that person an early diagnosis when treatment is more likely to be successful; and to do all this with 100% accuracy.
Although Alfattani’s research study is modest, her findings are potentially clinically relevant because they are on the Holy Grail therapeutic pathway, and her preliminary findings suggest that a simple, cheap and easy-to-use blood test - liquid biopsy - could detect breast cancer five years before any symptoms present. If demonstrated to be exquisitely accurate, safe and efficient by a larger study, which already is underway at Nottingham University’s CEAC, Alfattani’s research could be a key to saving thousands of lives and substantial amounts of money.
Alfattani was presenting research findings of a small study at the National Cancer Research Institute’s (NCRI) conference in Glasgow, Scotland, in November 2019, which is an international forum for showcasing cancer advances.
A September 2019 HealthPad Commentary described another early detection test for breast cancer called CanRisk, which has been developed by researchers from Cambridge University’s Centre for Cancer Genetic Epidemiology and has the potential to identify women with different levels of risk of breast cancer.
Alfattani and bioengineers from the universities of Nottingham and Cambridge are players in a vast and rapidly evolving international army of researchers engaged in an intensely competitive global race to develop an affordable, point-of-care, early detection test (EDT) for cancer based upon a liquid biopsy and next generation sequencing technologies. The Holy Grail is for such a test to detect cancer cells in an asymptomatic patient, locate the tissue of origin and give that person an early diagnosis when treatment is more likely to be successful; and to do all this with 100% accuracy.
Although Alfattani’s research study is modest, her findings are potentially clinically relevant because they are on the Holy Grail therapeutic pathway, and her preliminary findings suggest that a simple, cheap and easy-to-use blood test - liquid biopsy - could detect breast cancer five years before any symptoms present. If demonstrated to be exquisitely accurate, safe and efficient by a larger study, which already is underway at Nottingham University’s CEAC, Alfattani’s research could be a key to saving thousands of lives and substantial amounts of money.
Gold standard breast cancer screening
Currently, mammography screening is the gold standard for preventing and controlling breast cancer, which is costly to administer and only has a sensitivity between 72% and 87%. For every death from breast cancer that is prevented by mammography screening, it is estimated there are three false-positive cases detected and treated unnecessarily. Further, nearly half of all cancer sufferers are diagnosed late, when their tumours have already metastasized. It is estimated that 30% to 40% of cancer deaths could be prevented by early detection and treatment.
In this Commentary
This Commentary provides a partial update of some bioengineering initiatives described in a 2016 HealthPad Commentary, to speed up and improve liquid biopsies, which can simultaneously detect cancer early and identify its tissue of origin. Although there have been significant developments, the challenge for liquid biopsy assays still remains the level of their positive predictive values. This Commentary provides a brief and partial epidemiology of breast cancer, describes Alfattani’s research and its findings and briefly mentions some similar research that is underway. We describe categories of biomarkers employed by researchers and indicate some advances in EDTs made by some giant biopharma companies as well as briefly describing another innovative university-based development. We conclude by suggesting that: (i) despite significant and well supported research endeavours over the past decade to develop EDTs, there still remains a gap between scientific aspirations and reality; and (ii) there appears to be a gap opening between commercially available personalised cancer therapies, which are by-products of EDT research and standard oncological therapies.
Partial epidemiology of breast cancer
Despite significant advances in the awareness, diagnosis and treatment of breast cancer, it still remains the most common cancer in women worldwide, contributing 25.4% of the total number of new cases of cancer diagnosed in 2018. Each year, more than 0.5m women throughout the world die from the condition. In the US each year, over 268,000 new cases of invasive breast cancer are diagnosed in women, and over 41,000 women die from breast cancer. Between 1989 and 2016, death rates from female breast cancer in the US dropped by 40%. Over the past decade, death rates from breast cancer in older women in the US continued to decrease but remained steady in women under 50. Such decreases are attributed to increased awareness of the condition, earlier detection through screening and improved treatments. In the UK, there are over 55,000 new breast cancer cases diagnosed each year. In contrast to the US, since the early 1990s, breast cancer incidence rates in the UK have increased by around 19%, but death rates have fallen because of greater awareness, earlier detection and enhanced therapies. Notwithstanding, each year more than 11,000 women in the UK die from breast cancer. Furthermore, each year in the US, there are over 1.7m new diagnoses of all cancers, while in the UK there are over 360,000 new cases. Although recent advances in EDTs have the potential to decrease cancer deaths, as yet there is not a simple and cheap liquid biopsy, which can be used routinely in clinics to diagnose a range of cancers early. .
Alfattani’s research
The research pursued by Alfattani and her Nottingham colleagues is predicated upon the fact that cancer cells produce proteins called antigens, which trigger the body to make antibodies against them. These are called “autoantibodies”. Researchers discovered that these tumour-associated antigens (TAAs) are good indicators (biomarkers) of cancer. Alfattani and her colleagues developed panels of TAAs, which are known to be linked with breast cancer as a technique to detect whether or not there are autoantibodies against them in blood samples taken from patients.
The Nottingham researchers took blood samples from 90 breast cancer patients at the time they were diagnosed with the disease and matched them with samples taken from 90 patients without breast cancer (the control group). Researchers employed technology (protein microarray), which allowed them to screen the blood samples for the presence of autoantibodies against 40 TAAs associated with breast cancer and also 27 TAAs not known to be linked with the disease. The accuracy of the test improved in the panels that contained more TAAs.
The Nottingham researchers took blood samples from 90 breast cancer patients at the time they were diagnosed with the disease and matched them with samples taken from 90 patients without breast cancer (the control group). Researchers employed technology (protein microarray), which allowed them to screen the blood samples for the presence of autoantibodies against 40 TAAs associated with breast cancer and also 27 TAAs not known to be linked with the disease. The accuracy of the test improved in the panels that contained more TAAs.
Findings
A panel of five TAAs correctly detected breast cancer in 29% of the samples from the cancer patients and correctly identified 84% of the control group as being cancer-free. A panel of seven TAAs was able to detect disease in 35% of cases with breast cancer and rule out 79% of patients in the control group. The most successful technique was a panel of nine antigens, which correctly identified the disease in 37% of cancer samples and no cancer in 79% of the controls. “The results of our study showed that breast cancer does induce autoantibodies against panels of specific tumour-associated antigens. . . . . The results are encouraging and indicate that it is possible to detect a signal for early breast cancer. Once we have improved the accuracy of the test, then it opens the possibility of using a simple blood test to improve early detection of the disease”, said Alfattani.
David Crosby, head of early detection at the Cancer Research UK charity, said, “Diagnosing cancer at the earliest stages before it grows or spreads gives patients the best chance that their treatment will be successful. So, the potential to detect markers in the blood before other signs appear is promising”.
|
|
|
|
Directory:
Tags:

- Prime editing devised by researchers at the Broad Institute led by David Liu is a significant advance of the original CRISPR gene editing tool discovered in 2012
- CRISPR can cut and edit your DNA to correct defects inside your body’s cells to prevent and heal a range of incurable diseases and has revolutionized biomedicine
- The original CRISPR is fraught with inaccuracies referred to as off target effects
- Prime editing substantially reduces CRISPR’s off target effects and has the potential to correct up to 89% of known disease-causing genetic variations
- CRISPR also has the capacity to edit genes in an embryo in such a way that the change is heritable
- In 2018 Chinese researcher He Jiankui “created” the world’s first CRISPR babies
- This triggered international criticism from scientists and bioethicists
- A principal concern is that CRISPR is easy-to-use, cheap, regularly used in thousands of laboratories throughout the world and there is no internationally agreed and enforceable regulatory framework for its use
For better or worse we all now live in CRISPR’s world
In 2012 the world of biomedicine changed when a revolutionary gene editing technology known as CRISPR-Cas9 (an acronym for Clustered Regularly Interspaced Short Palindromic Repeats) was discovered. The technology harnesses your body’s naturally occurring immune system that bacteria use to fight-off viruses and has the potential to forever change the fundamental nature of humanity. Since its discovery CRISPR has been developing at lightning speed primarily because it is simple and affordable and today is used in thousands of laboratories throughout the world.
In this Commentary
In this Commentary we describe prime editing, which is the latest advance of the CRISPR's tool box, devised bya team of researchers, led by Andrew Anzalone, a Jane Coffin Childs postdoctoral fellow from the Broad Institute of MIT and Harvard and published in the October 2019 edition of Nature. Prime editing is significant because it provides a means to eliminate the unintentional consequences of CRISPR and therefore bring the technique closer for use in clinics. But this is still a long way off.
We also review a case where an ambitious scientist “created” the first CRISPR babies. This immediately triggered international criticism and a call for tighter regulatory control of the technology. Scientists and bioethicists are concerned that CRISPR can easily be used to create heritable DNA changes, which ultimately could lead to ‘designer babies’.
These two accounts of CRISPR might seem “opposites” and not sit well together in a single Commentary. Notwithstanding, what prompted putting them together was John Travis, the News Managing Editor of the well-known scientific journal Science, who soon after CRISPR’s discovery in 2012 said, “For better or worse we all now live in CRISPR’s world”.
CRISPR and your DNA
CRISPR is different to traditional gene therapy, which uses viruses to insert new genes into cells to try and treat diseases and has caused some safety challenges. CRISPR, which avoids the use of viruses, was conceived in 2007 when a yogurt company identified an unexpected defence mechanism that its bacteria used to fight off viruses. Subsequent research made a surprising observation that bacteria could remember viruses. CRISPR has been likened to a pair of microscopic scissors that can cut and edit your DNA to correct defects inside your body’s cells to prevent and heal a range of intractable diseases. The standard picture of DNA is a double helix, which looks similar to a ladder that has been twisted. The steps in this twisted ladder are DNA base pairs. The fundamental building blocks of DNA are the four bases adenine (A), cytosine (C), guanine (G) and thymine (T). They are commonly known by their respective letters, A, C, G and T. Three billion of these letters form the complete manual for building and maintaining your body, but tiny errors can cause disease. For example, a mutation that turned one specific A into a T results in the most common form of sickle cell disease.
We also review a case where an ambitious scientist “created” the first CRISPR babies. This immediately triggered international criticism and a call for tighter regulatory control of the technology. Scientists and bioethicists are concerned that CRISPR can easily be used to create heritable DNA changes, which ultimately could lead to ‘designer babies’.
These two accounts of CRISPR might seem “opposites” and not sit well together in a single Commentary. Notwithstanding, what prompted putting them together was John Travis, the News Managing Editor of the well-known scientific journal Science, who soon after CRISPR’s discovery in 2012 said, “For better or worse we all now live in CRISPR’s world”.
CRISPR and your DNA
CRISPR is different to traditional gene therapy, which uses viruses to insert new genes into cells to try and treat diseases and has caused some safety challenges. CRISPR, which avoids the use of viruses, was conceived in 2007 when a yogurt company identified an unexpected defence mechanism that its bacteria used to fight off viruses. Subsequent research made a surprising observation that bacteria could remember viruses. CRISPR has been likened to a pair of microscopic scissors that can cut and edit your DNA to correct defects inside your body’s cells to prevent and heal a range of intractable diseases. The standard picture of DNA is a double helix, which looks similar to a ladder that has been twisted. The steps in this twisted ladder are DNA base pairs. The fundamental building blocks of DNA are the four bases adenine (A), cytosine (C), guanine (G) and thymine (T). They are commonly known by their respective letters, A, C, G and T. Three billion of these letters form the complete manual for building and maintaining your body, but tiny errors can cause disease. For example, a mutation that turned one specific A into a T results in the most common form of sickle cell disease.
The original CRISPR
The original CRISPR tool, which is the first and most popular gene editing system, uses a guide RNA (principally a messenger carrying instructions from your DNA for controlling the synthesis of proteins) to locate a mutated gene plus an enzyme, like Cas9, to cut the double-stranded gene helix and create space for functioning genes to be inserted. However, a concern about CRISPR is that the editing could go awry and cause unintended changes in DNA that could trigger health problems. Findings of a study published in the July 2018 edition of the journal Nature Biotechnology found that such inaccuracies, referred to as off-target effects, were substantially higher than originally reported and some were thought to silence genes that should be active and activate genes that should be silent. These off-target effects, such as random insertions, deletions, translocations, or other base-to-base conversions, pose significant challenges for developing policy associated with the technology.
Subsequently however, the paper was retracted, and an error correction was posted on a scientific website. Contrary to their original findings, the authors of the Nature Biotechnology paper restated that the CRISPR-Cas9 gene editing approach, "can precisely edit the genome at the organismal level and may not introduce numerous, unintended, off-target mutations".
Notwithstanding, researchers remained concerned about CRISPR’s off target effects and several devised a technique, referred to as base editing, to reduce these. Base editing is described in three research papers published in 2017: one in the November edition of the journal ‘Protein and Cell’, another in the October edition of ‘Science’ the and a third by researchers from the Broad Institute, in the October edition of the journal ‘Nature’. Base editing takes the original CRISPR-Cas9 and fuses it to proteins that can make four precise DNA changes: it can change the letters C-to-T, T-to-C, A-to-G and G-to-A. The technique genetically transforms base pairs at a target position in the genome of living cells with more than 50% efficiency and virtually no detectable off-target effects. Despite its success, there remained other types of point mutations that scientists wanted to target for diseases.
Subsequently however, the paper was retracted, and an error correction was posted on a scientific website. Contrary to their original findings, the authors of the Nature Biotechnology paper restated that the CRISPR-Cas9 gene editing approach, "can precisely edit the genome at the organismal level and may not introduce numerous, unintended, off-target mutations".
Base editing
Notwithstanding, researchers remained concerned about CRISPR’s off target effects and several devised a technique, referred to as base editing, to reduce these. Base editing is described in three research papers published in 2017: one in the November edition of the journal ‘Protein and Cell’, another in the October edition of ‘Science’ the and a third by researchers from the Broad Institute, in the October edition of the journal ‘Nature’. Base editing takes the original CRISPR-Cas9 and fuses it to proteins that can make four precise DNA changes: it can change the letters C-to-T, T-to-C, A-to-G and G-to-A. The technique genetically transforms base pairs at a target position in the genome of living cells with more than 50% efficiency and virtually no detectable off-target effects. Despite its success, there remained other types of point mutations that scientists wanted to target for diseases.
|
|
|
|



















